Introduction. Over the past 30 years there has been considerable technological advancements in flexible ureteroscopy (fURS), resulting in its widespread use in the diagnosis and treatment of upper urinary tract disease, mainly urolithiasis [1]. To date, a wide range of reusable flexible ureteroscopes (rURS) is available [2, 3]. However, several recent studies reported some disadvantages of rURS. These include the high cost of purchase and repair of reusable devices and expenses of some sterility related issues, where complete sterilization procedure can reduce scope’s lifespan [4]. Furthermore, outbreaks of healthcare-acquired infections may occur due to insufficient or incomplete sterilization of these endoscopes [5]. Recently, Ofstead el al have examined 16 ureteroscopes after manual cleaning and sterilization. Tests detected contamination on 100% of ureteroscopes (including hemoglobin, adénosine triphosphate, and protein) and microbial cultures were positive in 2 out of 16 of the samples that have been taken from the ureteroscopes [6]. Injuries and infections have also been attributed to contaminated or damaged ureteroscopes, including those with broken wires, plastic coatings, and linings [7].
To overcome some of these disadvantages of reusable material, the adoption of single-use flexible ureteroscopes (suURS) has been proposed [8]. However, we still lack official recommendations for the use of suURS, as well as clinical data that indicates a substantial benefit of single user over reusable scopes [9]. Some studies have compared features and clinical outcomes of suURS with rURS. Clinical efficacy data showed that suURS was comparable with rURS revealing no significant differences in overall success rates and stone free rates [10-13]. In addition, these studies found comparable perioperative complication rates between both type of ureteroscopes but focused on small cohorts of patients.
In our center, a mixed use is made between rURS and suURS (UscopePU3022, Zhuhai Pusen Medical Technology Company Limited, China) since January 2017. The aim of this study was to compare the overall 30-days postoperative complications rates, especially infectious complications, following fURS for urolithiasis according to the type of ureteroscope used, single-use or reusable, in a high-volume center.
Material & Method. This is a single-center, retrospective study which included consecutive fURS procedures performed for the treatment of urinary stones in our department. Study cases included consecutive flexible ureteroscopic procedures in which UscopePU3022™ was utilized between January 2017 and May 2019. Study controls included consecutive cases in which reusable fiber-optic flexible ureteroscopes (3 fibered and 2 numeric rURS) were utilized during the same period. Single use ureteroscopes were used in case of unavailability of a reusable flexible ureteroscope (breakdown or repair) or in case of unavailability of the sterilization service. Patients’ demography, preoperative clinical characteristics, perioperative data and overall 30-days postoperative complications classified according to Clavien-Dindo grading system [14] were recorded from the patients’ charts. Data collection and study design were approved by the Ethics Committee of the Association Française d’Urologie (CERU_2019/013).
Preoperative evaluation included urine culture, complete blood count, renal function, electrolyte determination, and non-enhanced computed tomography (CT). Preoperative urine culture results were available 10 days before endoscopic surgery. A single dose prophylactic IV antibiotics was administered 30 min before the intervention in case of negative urine culture. In the absence of recommendations, our local protocol drawn up in collaboration with the infectious disease specialists provided for the administration of Ceftriaxone 48 hours before the start of the intervention in case of polymicrobial urine culture. In case of positive urine culture, antibiotic therapy was based in the culture-antibiogram test results and administered for 5 days before the intervention.
Ureteroscopy technique was standard. Retrograde pyelogram was systematically performed. In all cases the same brand of reinforced ureteral access sheath was used to allow passage of the digital scope. After inspecting the collecting system, lithotripsy was done using the Holmium laser system with a 200 to 365-µm fiber to disintegrate the calculi into fragments less than 2 mm under direct visualization. A Nitinol stone basket was used to remove large calculi fragments while small calculi fragments (<2 mm) were left in situ for spontaneous evacuation. After each procedure, reusable ureteroscopes undergoes a first treatment in the operating room: wiping, aspiration, and leak test. The second step of ureteroscope processing (sterilization and repacking) is carried out in the sterilization room, which involves: brush cleaning, rinsing, desinfection by soaking in peracetic acid, drying, and reconditioning.
The primary endpoint was occurrence of 30-days postoperative complications, especially infectious complications, classified according to Clavien-Dindo grading system [14]. Statistical analysis was performed with R® version 3.5.3 using the chi-square test or Fisher’s exact test for nominal variables and the Mann-Whitney test for continuous variables. Statistical significance was considered at p<0.05.
Results. Overall, 322 consecutive fURS were included between January 2017 and May 2019 corresponding to 186 rURS (57.8%) and 136 suURS (42.2%). Baseline characteristics were comparable between both groups (Table 1). Respectively in rURS and suURS groups, the median (IQR) age was 57 (45-65) vs 57 (44-66) years (p=0.75), 83 (44.6%) vs 63 (46.3%) female were included (p=0.82), and median (IQR) Charlson score was 2 (1-3) vs 2 (0-3) (p=0.15). Patients were not systematically pre-stented. Overall, 249 of the 322 patients (77.3%) had a JJ stent placed before endoscopic surgery (rURS group: 147 [79%] vs suURS group: 102 [75%]; p=0.39). Preoperative double-j stents were inserted in cases with history of complicated urinary tract infection (UTI) or for passive ureteral dilation to facilitate insertion of the ureteral access sheath. All patients had a preoperative urine culture, most of them being sterile (66.1%). Results of preoperative urine culture were also comparable between both groups (p=0.67).
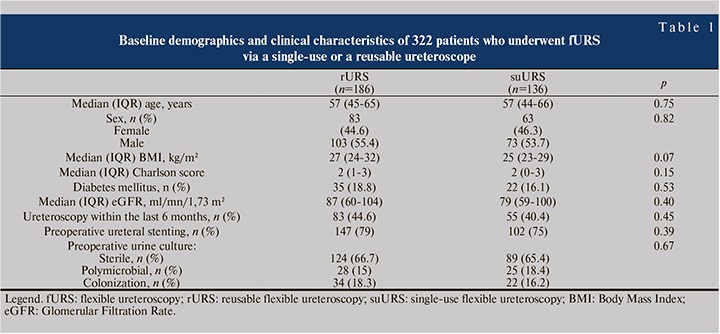
Table 2 shows the ureteroscopy procedures characteristics. All interventions were indicated for the treatment of urinary stone. A kidney stone larger than 20 mm in its longest axis, defined on the preoperative CT-scan, was reported in 70 (37.6%) and 49 (36%) cases, respectively in rURS and suURS groups (p=0.76). However, the composition of the lithiasis was not known. Ureteral access sheath was systematically used. Median (IQR) operative time was 60 (45-79) and 60 (45-76) min (p=0.60), respectively in rURS and suURS groups. Postoperative ureteral stenting was common in each group and was performed in 311 (96.5%) cases in overall cohort (p=0.21).
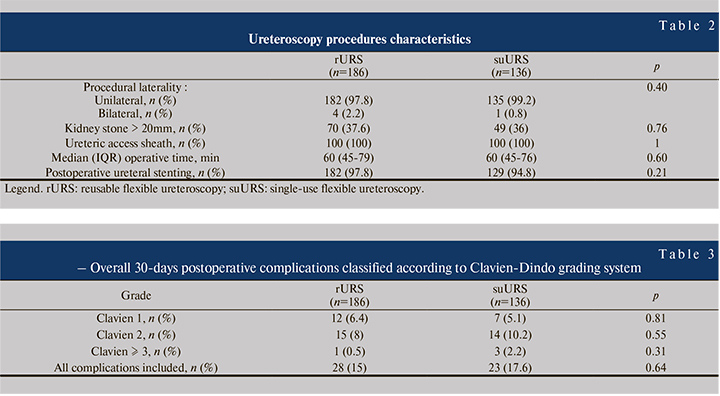
Table 3 shows overall 30-days postoperative complications classified according to Clavien-Dindo grading system. Of the included 322 patients, 51 patients (15.8%) developed postoperative complication, 28 patients (15%) in rURS group and 23 patients (17.6%) in suURS group, without statistical difference in minor (Clavien 1-2; p=0.81) or major (Clavien ≥ 3; p=0.31) complications between both groups. In rURS group, twelve Clavien 1 (11 cases of flank pain requiring anti-inflammatory drugs and 1 case that developed ileus), fifteen Clavien 2 (10 cases of upper UTI, 3 cases of hyperkalemia treated medically, 1 case of prolonged hematuria and 1 case of acute pancreatitis) and one Clavien ≥ 3 (urosepsis) complications were recorded. In suURS group, seven Clavien 1 (5 cases of flank pain requiring anti-inflammatory drugs, 1 case of bradycardia settled conservatively and 1 case of nausea), fourteen Clavien 2 (13 cases of upper UTI and 1 case of stable angina) and three Clavien ≥ 3 (3 cases of urosepsis) complications were recorded. Injury of the upper urinary tract during ureteroscopy procedure was not observed in either group.
Of the included 322 patients, 23 patients (7.1%) developed postoperative UTI, 10 cases (5.4%) in rURS group and 13 cases (9.5%) in suURS group (p=0.15). UTI occurred in a median (IQR) time of 2 (1-3) and 2 (1-3) days (p=0.91), respectively in rURS and suURS groups. Urosepsis occurred in 4 cases including one death due to septic shock. Regarding preoperative bacterial ecology of the patients with UTI, in rURS group and suURS group respectively, 30% (3 of 10) and 23% (3 of 13) had preoperative urine culture with no growth, 50% (5 of 10) and 46% (6 of 13) had preoperative polymicrobial urine culture, 20% (2 of 10) and 31% (4 of 13) had antibiotics during 5 days before the intervention for a positive preoperative urine culture (p=0.99). Ten of twenty three patients with UTI showed a postoperative positive result of urine culture without any significant difference in both groups (p=1). Cultures were identified to be Pseudomonas aeruginosa and Enterococcus spp. in 4 patients each, Escherichia coli and Candida spp. in 1 case each.
Discussion. During the past decade, several suURS were introduced in some countries in an attempt to offer a reliable, clinically non inferior and cost-effective alternative. A number of suURS are now available for commercial use (Polyscope™, SemiflexM, FlexorVue™, Neoflex™, Lithovue™, and UscopePU3022™). However, there are still a lack of clinical data comparing the safety between single-use and reusable fURS [12]. We therefore conducted a retrospective and comparative study of 30-days postoperative complications between rURS and suURS (UscopePU3022™, Zhuhai Pusen Medical Technology Company Limited, China).
Flexible ureteroscopy, in addition to its widely applicable diagnostic and therapeutic benefits, may be associated with noticeable complications, most of which are Clavien grade I or II [15]. Few studies has evaluated postoperative complications after performing suURS and had contradicting results. Usawachintachit et al [10], which compared LithoVue™ (Boston Scientific, Marlborough, MA) and rURS, reported that LithoVue™ was significantly associated with lower postoperative complication rate than Olympus P6 (p<0.05). Authors concluded that these difference was possibly reflective of the study design rather than a factor intrinsically related to the ureteroscopes. Conversely, Mager et al [11] and Kam et al [13] did not report a significant difference in complication rates after performing ureteroscopy. Compared to previous studies, our series which represents the largest cohort of patients, supports that the overall postoperative complication rate is comparable between suURS and rURS.
Ureteroscopy requires direct contact between a surgical device and a patient’s tissues. To limit the transmission of infectious agents, disinfection of the surgical equipment is a must after each procedure. If endoscopes do not attain a sufficiently high level of sterilization, they may cause cross contamination. Indeed, outbreaks of healthcare-acquired infections have been linked to duodenoscopes, gastroscopes, bronchoscopes and cystoscopes [16-20]. Injuries and infections have also been attributed to contaminated or damaged ureteroscopes, including those with broken wires, plastic coatings, and linings [7]. A recent ex vivo chemical analysis of ureteroscopes at two large multispecialty academic centers in the midwestern United States detected microbial growth on 13% of sterilized instruments and protein on 100% of devices [6]. Investigators attributed these findings to structural irregularities, discoloration, and damage to the ureteroscope working channel [6]. However, clinical impact of using contaminated ureteroscope was not evaluated. These findings support the use of disposable instruments to avoid cross-contamination of rURS. However, in a real-world study, we reported that the use of rURS was not associated with an increased risk of postoperative UTI. Although microbial cultures of reusable ureteroscopes after sterilization was not performed, we did not detect a clinically significant impact of a potential cross-contamination of rURS. Our results are supported by a recent study where authors evaluated in 389 ureteroscopy procedures the effectiveness of high level disinfection with peracetic acid [21]. Pre-use ureteroscope cultures were positive in 47 of 389 procedures (12.1%), of which uropathogens were found in 9 of 389 (2.3%) and skin flora in 38 of 389 (9.8%). Urinary tract infection symptoms did not develop in any of the patients who underwent surgery with a uropathogen contaminated ureteroscope [21].
There are some limitations in this study. First, the main limitation is its retrospective design. Second, our center used the suURS UscopePU3022™ and the results may not be applicable to other types of disposable devices. Third, no microbiological analysis of the rURS was performed before and after the procedure and a prospective evaluation would be very interesting to perform.
Conclusion. In conclusion, we reported a case control study of a large single center experience with UscopePU3022™. Our data suggest that suURS represents a safe alternative to rURS. Compared to reusable devices, UscopePU3022™ use was associated with a similar complication rates, however, did not decrease the occurrence of infectious events.
Declaration
Funding: none
Conflicts of interest: no
Ethics approval: Data collection and study design were approved by the Ethics Committee of the Association Française d’Urologie (CERU_2019/013)
Consent to participate: Not applicable
Consent for publication: Not applicable
Availability of data and material: yes
Code availability: yes
Study concept and design: Baboudjian, Boissier and Lechevallier. Acquisition of data: Baboudjian. Analysis and interpretation of data: Baboudjian, Gondran-Tellier, Boissier and Lechevallier. Drafting of the manuscript: Baboudjian, Boissier, Lechevallier. Critical revision of the manuscript for important intellectual content: Karsenty, Lechevallier. Statistical analysis: Gondran-Tellier. Administrative, technical, or material support: Baboudjian, Boissier, Lechevallier, Gondran-Tellier, Akiki, Abdallah, Gaillet, Delaporte and Karsenty.