Introduction
According to publication by Yaxley JPC., in 2016 [1], cancers of urinary system are common and include a series of injuries encompassing from small benign tumors to destructive neoplasms with high morbidity. The urinary tract is lined by epithelium extending from the renal accumulating tubules proximally to the external urethral orifice distally. These epithelial cells are recognized as the urothelium or transitional cells. They are highly specialized cells with elasticity and variable shape. Any segment of the urothelium can be affected by malignant transformation. According to Globocan data, globally, in the year 2008, 12.7 million newly developed cases with cancer, and 7.6 million cancer-related deaths were detected [2]. Siegel R, et al., in 2013 reported [3]] that advanced urothelial carcinoma accounts for about 15,000 deaths in the United States annually. The most common malignancy reported as urinary bladder cancer. Upper tract urothelial carcinoma is more common in men than in women, with a male-to-female ratio of 2:1. The main risk factors are occupational exposure, various chemical carcinogens and cigarette smoking. [4] Histological tumor classifying is an established predictive factor of renal cell carcinoma [5]. Citologically and histologically, overexpression of p16INK4a has been recognized in urothelial malignancies. Therefore, there are potential implications for the clinical management of patients after the conservative treatment of non-muscle-invasive urothelial carcinoma. Furthermore, a long-term assessment of p16/Ki-67 double labeling has been revealed to distinguish high-grade urothelial cancer cells and particular development individuals within a 12-month interruption [6]. In population with clear-cell renal cell carcinoma collecting system invasion is related with deprived prediction [7]. Total existence and progression-free survival in patients with urinary system cancer could be associated to high serum of lactate dehydrogenase, and therefore it is an effective biomarker of prognosis in patients with urologic cancer [8]. Study of kidney cancer in rural Illinois showed that kidney and renal pelvis cancer incidence was higher in urban counties whereas mortality was higher in rural counties [9] Urological malignancy was accounted for 9.55% of new cases of cancer in 2012 in Hong Kong [10]. Study of 198 patients with BC and 396 healthy individuals in Shiraz/Iran confirmed that opium consumption can be a potential strong risk factor for BC in Iran [11]. Therefore the aim of this study was to show up-to-date estimates of crude rate, incidence rates and differences in rates between men and women of urinary system cancer in Isfahan/Iran.
Patients and Methods
This study was conducted to the Isfahan Kidney Transplantation Research Center (IKTRC) and approved by the Isfahan Deputy of Research Committee via the Ethics Committee Code Number of 295115. Cancer data obtained from Isfahan Cancer Registry located in deputy of health. Data considered in this study belonged to the years between March 2011 to March 2015. The cancer sites studied were characterized according to the International Classification of Diseases (ICD-O; Third Edition). All cancers were defined by topography code. For example kidney was defined by topography code C64, renal pelvis by topography code C65, ureter by topography code C66 and bladder by topography code C67. De-identified patient name and surname, demographic such as age and gender, final code for cancer diagnosis and date of reported cancer were recorded. Variables such as gender, alive/dead, year of report were expressed by frequency, percentage, period prevalence and incidence rate. The total population for Isfahan City was obtained from the Isfahan/Program and Budget Management Organization. Period Prevalence was calculated as the proportion of total cases over the period of the years 2011-2015/ to population at risk during the same time period x 100000. Cancer Incidence Rate (CIR) was calculated as dividing new cases of cancer during a given time period / to population at risk during the same time period x 100000. Analysis of data was carried out using the Statistical Package for Social Science (SPSS® version 20 IBM Corp., Armonk NY, USA). Age that was a continuous variable was expressed by mean ±standard deviation (SD) [12, 13].
Results
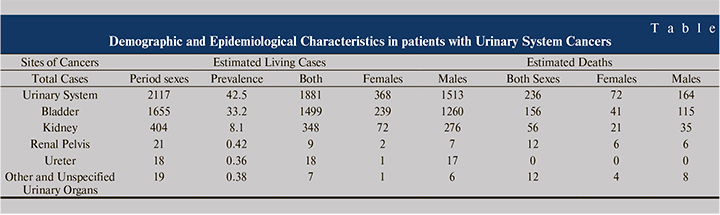
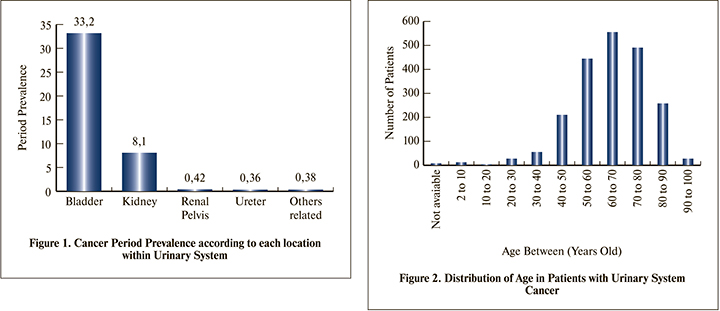
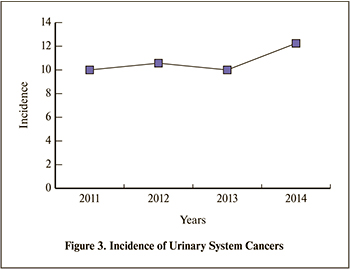
Table 1 shows demographic and epidemiological characteristic in 2117 patients with urinary system cancers. The study population comprised of 440 females and 1677 males. The total period prevalence was calculated as 42.5 per 100000 persons (Figure 1) that were corresponded to: 33.2 for bladder, 8.1 for kidney, 0.42 for renal pelvis, 0.36 for ureter and 0.8 for other and unspecified urinary organs. With the mean age±standard deviation of 63.6±14.9 years old, age related to urinary system cancers in 1%, 62% and 37% were related to age under 20, between 20 to 70 and 70 to 100 years old of life respectively (Figure 2). Death reported-data was associated to 11% of total cases. The rate of males to females was 83% for bladder, 77% for kidney, 62% for renal pelvis, 94% for ureter and 74% for other and unspecified urinary organs. Incidences of urinary system cancer were calculated as: 9.9 (2011 to 2012), 10.5 (2012 to 2013), 9.9 (2013 to 2014) and 12.2 (2014 to 2015) per 100000 persons (Figure 3).
 Discussion
Discussion
Urinary system cancers are common and impose an important cost weight on health system. Previous publication reported that urinary bladder and kidney cancers are the most frequent malignant tumors of the urinary system, together making up to 5% of all cancers worldwide [14]. As there has been little information associated to incidence trends of urinary system in Iranian/Isfahan population, therefore this study conducted an analysis on urinary system cancers data from the population-based Cancer Registry.
In agreement with previous study of Western countries in which specified an increasing trend toward incidence of urinary bladder and kidney cancers [15], in this study incidence of urinary system cancers 23.2% was increased between 2011 and 2015. Previous publication confirmed that regarding to Iranian population, there is a shift to older-in-age distribution that has begun in developing countries including in Iran [16]. In agreement with previous publication that mentioned the mean age of diagnosis of 65 years [17], in this study also the mean age of patients was also 63.6 years old.
The result of this study is in agreement with the Australian Institute of Health and Welfare report that confirmed bladder cancer as the most common cancers with a rise in incidence [18]. Prithwish De et al., in 2014 studied [19], incidence of kidney cancer between 1986 and 2007. The age-standardized incidence rate per 100,000 rose from 13.4 to 17.9 in males and 7.7 to 10.3 in females. In this study the period prevalence was ranked for bladder cancer with a value of 33.2 and 8.1 for kidney per 100000 persons correspondingly. The period prevalence was significantly different between males and females (66.4 vs 17.9 p<0.001) respectively.
The estimated deaths were correlated to 236 out of 2117 (11.1%) patients with urinary system cancers. Reported mortality in cancer of renal pelvis was associated to 57.2% and this is in agreement with published report from Bailey GC, et al in 2017 that mentioned collecting system invasion is associated with poor prognosis among patients with clear-cell renal cell carcinoma [6]. Finally the results of this study showed that urinary bladder, kidney cancer followed an increasing trend in incidence, mortality and prevalence in Isfahan/Iran. Finally research practice points confirmed that: 1) Health care system should provide model-base-strategy to improve access to specialized medical, pharmacological and surgical facilities 2) Consideration needed toward the reality for scheduling health system improvements, particularly referral systems 3) Preventing of significant difficulties by management equality for patient satisfaction 4) Attention toward financial management by study of epidemiology and pharmacoepidemiology.
Conclusion
From the year 2011 to 2015 there were 2117 patients with urinary system cancers in Isfahan Province. The mean age ± SD was 63.6±14.9 years old. In the 62% of total population age ranged between 20 and 70 years old. The period prevalence for total population was 42.5 per 100000 persons. Total period prevalence was corresponded to 66.4 per 100000 males and 17.9 per 100000 females (p<0.001). The period prevalence was 33.2 for bladder, 8.1 for kidney, 0.42 for renal pelvis, 0.36 for ureter and 0.38 for other unspecified related organs. There were living cases comprised of 368 females and 1513 males. There was 23.2% increase in the Irs over the study period. For future plan associated to such populations’ further research toward oncology drugs used in Iran recommended.
Acknowledgement
Thanks to Isfahan University of Medical Sciences with Ethical Code No 295115 appreciated