Введение. Крипторхизм – самая частая аномалия развития мужских гениталий, встречающаяся примерно у 1,1% мальчиков в возрасте 1 года [1]. Среди всех форм крипторхизма на долю непальпируемых яичек приходится 20–27% [2, 3], из них истинно интраабдоминальные формы крипторхизма, в том числе и яички, расположенные у внутреннего пахового кольца, составляют, по разным данным, от 45,6 до 72,6% [3–7].
Принципы хирургического лечения абдоминальных форм крипторхизма (АФК) заложены в 1959 г. Stephens и Fowler [8], обосновавшими возможность пересечения тестикулярных сосудов с целью устранения ограничений по длине элементов семенного канатика при низведении яичка в мошонку. Их исследование предопределило дальнейшее развитие хирургии АФК, и за прошедшие полвека удалось снизить частоту послеоперационной тестикулярной атрофии с 33,3 [8] до 15,0% [9]. Одним из итогов развития хирургической тактики при лечении непальпируемых форм крипторхизма стало формирование лечебного алгоритма, при котором стартовой процедурой является диагностическая лапароскопия (ДЛ) [10–12].
Z. Laron и E. Zilka в 1969 г. впервые описали феномен гипертрофии здорового яичка [13], являющейся физиологическим ответом на отсутствие или значительное недоразвитие ретенированного яичка. В 1991 г. S. Koff [14] отметил, что тестикулярная гипертрофия возникает в возрасте от 8 мес. до 13 лет, и установил, что объем здорового яичка более 2 мл в значительной мере стновится предиктором монорхизма.
В 2004 и 2007 гг. W. Snodgrass et al. предложили скрототомию в качестве первичного доступа с целью снижения количества неоправданно выполняемых ДЛ пациентам с непальпируемыми формами крипторхизма. В работе 2004 г. [15] исследователи выявляли наличие компенсаторной тестикулярной гипертрофии (объем более 2 мл), но не ставили своей задачей ее использование в качестве диагностического критерия. Позднее, в 2007 г. [16], они отметили, что при выявлении размера здорового яичка более 1,8 см скрототомия является предпочтительным первичным доступом.
 C учетом необходимости снижения частоты выполнения неоправданных лапароскопий целью данного исследования стал расчет пороговых значений объема контралатерального яичка при одностороннем непальпируемом крипторхизме, позволяющий оптимизировать диагностику и тактику хирургии.
C учетом необходимости снижения частоты выполнения неоправданных лапароскопий целью данного исследования стал расчет пороговых значений объема контралатерального яичка при одностороннем непальпируемом крипторхизме, позволяющий оптимизировать диагностику и тактику хирургии.
Материалы и методы. С 2010 по 2016 г. ДЛ выполнена 192 пациентам с 222 непальпируемыми яичками, среди которых левосторонний крипторхизм выявлен у 89 (46,4%), правосторонний – у 73 (38,0%), билатеральное поражение – у 30 (15,6%) мальчиков. Абдоминальная ретенция выявлена в 108 (47,3%) наблюдениях, в 68 (30,6%) – определены значительно гипоплазированные яички или выявлено их отсутствие (аплазия, атрофия). Сорок шесть (20,7%) гонад обнаружены в паховом канале и 3 (1,4%) были эктопированы. Из исследования исключены пациенты в возрасте старше 9 лет с предшествовавшим курсом гормонотерапии, с двусторонним крипторхизмом и мальчики, у которых утеряна информация о предоперационном объеме здорового яичка. В итоге в исследование включены 78 (39,6%) пациентов, в зависимости от состояния крипторхического яичка разделенных на две группы. В 1-ю группу вошли пациенты с паховыми (ПЯ) или интраабдоминальными (ИАЯ) яичками, которым выполнено низведение выявленных гонад, во 2-ю – пациенты с резко гипоплазированными яичками, требовавшими удаления, или те, у которых яичко отсутствовало (аплазия). Средний возраст пациентов на момент проведения оперативного лечения составил 36,4 мес. (Me – 24 мес. [Q1 – 19 мес.; Q3 – 48 мес.]).
С помощью линейки всем пациентам измерили длину, ширину и глубину контралатерального яичка, объем вычислили по формуле:
Vяичка = длина×ширина×высота×0,71.
Статистический анализ и обработку собранных данных выполнили в R (версия 3.2, R Foundation for Statistical Computing, Австрия). В качестве описательных статистик использованы средние значения, стандартные отклонения, медианы и квартильный размах (Me [Q1; Q3]). Сравнение медиан в группах проведено с помощью теста Манна–Уитни. Для построения диагностической модели применяли логистическую регрессию. Анализировали значимость коэффициентов регрессии, для регрессора оценивалось отношение шансов (OR) и 95% доверительный интервал (95% CI).
Для модели строили ROC-кривую и выбирали пороговый уровень, соответствовавший лучшему сочетанию чувствительности и специфичности.
Критическое значение уровня статистической значимости при проверке нулевых гипотез приняли равным 0,05.
Результаты. Среди 41 ребенка 1-й группы яички располагались абдоминально у 24 (58,5%) и в паховом канале у 17 (41,5%). Во 2-й группе у 25 (67,6%) пациентов выявлено резко гипоплазированное яичко и в 12 (32,4%) наблюдениях – отсутствие гонады. На рис. 1 представлены объемы здоровых яичек пациентов обеих групп.
Как видно из таблицы, пациенты обеих групп были сопоставимыми по возрасту, но статистически значимо различались по объему контралатерального яичка (p<0,0001). Для объема контралатерального яичка коэфициент логистической регрессии составил -2,84,
OR [95% CI]: 0,06 [0,02; 0,2], уровень статистической значимости: р=0,00002.
Формула модели:
Вероятность обнаружения яичка, подлежащего низведению,=logistic (5,62–2,84*объем контралатерального яичка).
Для оценки качества модели был проведен ROC-анализ (рис. 2). Площадь под кривой (AUC) составила 92,6%, что говорит о высокой прогностической силе модели.
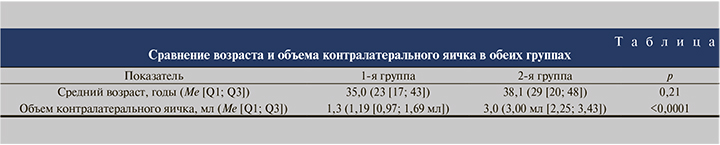
У всех пациентов с объемом здорового яичка, меньше или равным 1,04 мл, обнаружены ИАЯ или ПЯ, низведенные в мошонку. При пороговом уровне вероятности в 93,6% чувствительность составила 34%, специфичность – 100,0%.
У всех пациентов с объемом здорового яичка, более или равным 2,26 мл, яички либо отсутствовали (аплазия, атрофия), либо оказались резко гипоплазированными. При пороговом уровне вероятности в 31,5% чувствительность составила 100%, специфичность – 73%.
Обсуждение. Исходя из того, что при недоразвитии или удалении таких парных органов, как почки, надпочечники, яичники, у пациентов выявляется компенсаторная гипертрофия сохраненного органа, Z. Laron и E. Zilka в 1969 г. [13] первыми сообщили о контралатеральной тестикулярной гипертрофии при монорхизме. В их исследовании приняли участие 38 мальчиков с гипогонадизмом, из них 35 пациентов с односторонними и 3 – с двусторонними формами крипторхизма. Определяли объем яичек с использованием штангенциркуля и орхидометра (разработан A. Jaacob), а также длину и ширину полового члена. Помимо этого рассчитали скелетный возраст, определили уровень кетостероидов и гонадотропина. Объем яичка рассчитали по формуле Hansen & With: объем яичка=длина – 1 мм ×(ширина – 1 мм)2 × 0,52. При сопоставлении данных, полученных расчетным методом и с помощью орхидометра, значимых различий выявлено не было. Показатели нормального объема яичек, согласно данным литературы и собственным наблюдениям, были сопоставлены с объемами, полученными у испытуемых. Было обнаружено, что у детей с крипторхизмом объем здорового яичка (3,75 мл) значительно выше, чем в контрольной группе (1,64 мл). Кроме того, отмечено, что у пациентов с двусторонним крипторхизмом тестикулярная гипертрофия развивается у более полноценного яичка. По результатам наблюдений установлено, что тестикулярная гипертрофия здорового яичка полностью компенсирует недоразвитие или отсутствие контралатерального, свидетельством чего служат линейный рост, половое и скелетное развитие, а также нормальный уровень кетостероидов у всех пациентов.
В 1991 г. S. Koff [14] был первым, кто предложил пороговый уровень объема здорового яичка, позволяющий предсказывать состояние непальпируемого яичка или его отсутствие. Автором был сделан вывод, согласно которому степень гипертрофии зависит от трех факторов: 1) скорости снижения объема крипторхического яичка, 2) возраста, при котором возникло повреждение яичка, и 3) состояния опущенного яичка. В качестве инструмента, позволяющего измерить объем, автор использовал орхидометр Такихара. Установлено, что при размере яичка более 2 см (что соответствует объему 2 мл) хирургические мероприятия не позволят выявить ни нормальную, ни поврежденную тестикулярную ткань. При этом автор указывает на сравнительно малый объем выборки и считает необходимым изучить бóльшую выборку на предмет выявления иных, влияющих на возникновение компенсаторной гипертрофии факторов.
Вопреки этому исследованию D. Huff et al. [17] сообщили, что объем более 2 мл не является 100%-ным предиктором монорхизма, так как в их исследовании у 80% мальчиков с единственным здоровым яичком размер был менее 2 мл и, что немаловажно, у 1 пациента с абдоминальным, подлежащим низведению яичком объем здорового яичка превышал 2 мл. Однако, учтя разные методы определения объема, D. Huff et al. измерили размеры яичка штангенциркулем и вычислили объем по формуле эллипса Lambert: объем яичка=(4/3)π×(длина×ширина×высота), – сравнивать пороговые значения этих исследований не представляется возможным.
Эти работы послужили толчком к проведению исследований, посвященных компенсаторной гипертрофии опустившегося яичка. Так, в 2001 г. опубликована работа [18], основной задачей которого стала проверка предложенного Koff инструмента для диагностики монорхизма. В качестве такого инструмента использовали орхидометр Такихара и линейку. В тех ситуациях, когда с помощью линейки измерить длинник было невозможно, его определяли путем сопоставления объема, измеренного орхидометром, соответствующей ему длине яичка, помимо этого ученые регистрировали данные объективного осмотра. Всего в исследовании приняли участие 56 пациентов. Показано, что увеличение размера яичка до 1,8 см и более (31 мальчик) в 90,3% наблюдений служит показателем отсутствия непальпируемого яичка. Среди 41 пациента, у которых не определялись «смутно» пальпируемые структуры, с размером яичка более 1,8 см в 100% наблюдений выявлялся монорхизм.
H. Mesrobian et al. [19] учли наличие пальпируемых образований и объем яичек. Результатом исследования стал вывод, согласно которому отклонение объема здорового яичка более чем на 2 стандартных отклонения (97-й перцентиль) в большинстве случаев служит свидетельством отсутствия ИАЯ или ПЯ. Поскольку монорхизм выявлен всего у 13% пациентов, среди которых были 2 ребенка с размером яичка более 2 см, авторы пришли к заключению, что наличие пальпируемых образований является более значимым диагностическим критерием, нежели компенсаторная гипертрофия.
W. Snodgrass et al. [20] подняли вопрос о целесообразности выполнения ДЛ всем пациентам с непальпируемыми яичками и в качестве альтернативы предложили первично проводить ревизионную скрототомию. Тестикулярная гипертрофия выявлена у 15 (65,2%) из 23 пациентов с монорхизмом и у 2 пациентов с яичками, подлежащими низведению. Позже было показано [21], что размер яичка более 1,8 см, как и более 2,0 см, является предиктором монорхизма c 88%-ной вероятностью. У пациентов с яичками, требующими низведения, компенсаторная тестикулярная гипертрофия выявлена в 4 (9,3%) случаях (у 1 пациента размер составил 1,8–1,9 см и у 3 превысил 2,0 см).
Y. Shibata et al. [22] опубликовали работу, в которой у пациентов с односторонними непальпируемыми формами крипторхизма линейкой определяли размер и объем здорового яичка (формула вычисления объема в статье не представлена). В результате обнаружено, что при длине более 22,4 мм и объеме 2,2 мл наиболее вероятно отсутствие яичка (чувствительность/специфичность составили 81,8%/95,5% для длины и 84,8%/86,4% для объема).
L. Braga et al. [23], пользуясь штангенциркулем для измерения объема яичка, заключили, что при размере яичка 19–20 мм будет выявлен монорхизм. Чувствительность метода составила 97%, специфичность – 85%, что позволяет использовать этот диагностический критерий при выборе хирургического доступа.
A. Hodhod et al. [24], определив объем здорового яичка орхидометром Такихара, сделали вывод: при наличии компенсаторной гипертрофии здорового яичка более 2 мл в 100% случаев будет выявлено отсутствие яичка или его гипоплазия (чувствительность – 71,7%, специфичность – 100%).
В 2017 г. P. Shadpour et al. [25] опровергли все полученные ранее результаты об информативности компенсаторной гипертрофии у пациентов младше 18 лет. По их данным, полученным в результате определения размеров яичка с использованием ультразвукового исследования и расчета объема по формуле: длина×ширина×высота×0,71, статистически значимых различий в объеме здорового яичка у пациентов с ПЯ или ИАЯ и монорхизмом (отсутствие яичка, гипоплазия яичка) не найдено. Стоит отметить такую особенность, как регион проведенного исследования: все пациенты были жителями Ближнего Востока. Известно, что этническая принадлежность может влиять на тестикулярный объем у взрослых мужчин [26], поэтому, на наш взгляд, с учетом значительно отличающегося результата данное исследование необходимо воспринимать как основание для дальнейшего изучения тестикулярного объема в различных этнических группах.
Авторы всех представленных выше исследований использовали тестикулярный объем только с целью определения признаков монорхизма у пациентов с односторонним непальпируемым крипторхизмом. Нам представляется важным выделить группу больных, у которых тестикулярный объем может быть использован как критерий, указывающий на наличие ретенированного яичка. Эта группа пациентов, без всяких сомнений, нуждается в ДЛ.
Заключение. Оптимизация выбора стартовой хирургической процедуры для пациентов с односторонними непальпируемыми формами крипторхизма с целью исключения ненужных лапароскопий остается нерешенной проблемой. Результаты наших исследований позволяют утверждать, что ревизионная скрототомия показана во всех случаях при объеме тестикулярной ткани здорового яичка более или равном 2,26 мл, а диагностическая лапароскопия является единственно правильной стартовой процедурой для пациентов с объемом контралатерального яичка менее 1,04 мл.