Введение. Общепринятым фактором риска осложненного течения COVID-19 в настоящее время являются кардиометаболические заболевания: ожирение, сахарный диабет (СД), артериальная гипертензия (АГ), ишемическая болезнь сердца (ИБС) [1]. Помимо этого доказанным считается, что мужской пол способствует тяжелому течению COVID-19. Так, согласно мета-анализу, опубликованному в январе 2021 г., мужчины в 1,38 раза чаще попадают в отделение реанимации и интенсивной терапии с COVID-19 и в 1,5 раза чаще умирают [2].
Основа подобных гендерных различий связана, вероятнее всего, с генетическими и гормональными особенностями мужского и женского организмов. Так, в исследовании in vitro показано, что дигидротестостерон (ДГТ) способен увеличивать экспрессию сразу двух белков, необходимых для проникновения SARS-Cov-2 в клетки: ангиотензинпревращающего фермента 2 (АПФ2) и трансмембранной сериновой протеазы 2-го типа (TMPRSS2) [3].
Таким образом, логично предположить, что снижение концентрации ДГТ может оказывать защитное влияние в отношении заболеваемости COVID-19. В связи с этим проведено несколько исследований по изучению влияния андрогенной депривационной терапии (АДТ) на заболеваемость и тяжесть течения COVID-19. Одни работы показывают, что прием АДТ ассоциирован с меньшей заболеваемостью COVID-19 [4, 5]. По результатам других не было выявлено значимого влияния АДТ в отношении заболеваемости COVID-19 [6–8].
Однозначного ответа нет и в отношении взаимосвязи частоты госпитализаций и приема АДТ. В более ранних исследованиях продемонстрировано, что пациенты, принимающие АДТ, почти в 4 раза реже госпитализируются с COVID-19 [9], в то время как в многоцентровом исследовании, завершенном в 2022 г., прием АДТ не был ассоциирован с частотой госпитализаций и тяжестью течения COVID-19 [10], что подтверждено и в других работах [11].
Основным ограничением большинства проведенных исследований стало включение в выборки пациентов, принимающих различные типы АДТ без выделения одной конкретной группы препаратов, что может объяснять разнообразие результатов. Как известно, АДТ включает препараты, отличающиеся по механизму действия, которые могут по-разному влиять на концентрацию андрогенов [12]. Так, если агонисты и антагонисты гонадотропин-рилизинг-гормона (ГнРГ) обладают однонаправленным действием на концентрацию тестостерона (Т) и ДГТ, то антиандрогены могут оказывать диаметрально противоположный эффект в зависимости от структуры применяемого препарата. Другие представители АДТ, ингибиторы 5-альфа-редуктазы (5-АРИ), блокируют одноименный фермент, обеспечивающий конвертацию Т в ДГТ, и тем самым обеспечивают снижение концентрации ДГТ без изменения концентрации Т или даже с небольшим компенсаторным повышением последнего [12, 13]. Таким образом, возникает необходимость раздельного анализа влияния различных типов АДТ на заболеваемость и частоту госпитализации при COVID-19.
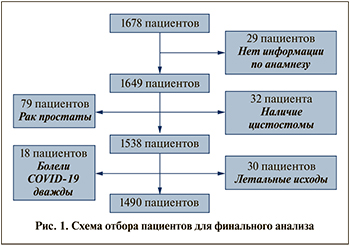
К наиболее распространенным препаратам, применяемым в качестве АДТ, относятся представители группы 5-АРИ, назначаемые при гиперплазии предстательной железы, встречающейся у 60% мужчин в возрасте 60 лет и у 90% мужчин старше 70 лет [14]. Таким образом, целью настоящего исследования стала оценка заболеваемости COVID-19 и частоты госпитализаций пациентов-мужчин с ГПЖ в зависимости от приема ингибиторов 5-альфа-редуктазы (5-АРИ). Материалы и методы. Исследуемая выборка. В ходе исследования проанализированы все последовательные электронные медицинские карты 1678 пациентов, наблюдавшихся амбулаторно с диагнозом «гиперплазия простаты» с 01.2020 по 01.04.2022. Собрана информация о возрасте пациента, индексе массы тела (ИМТ), наличии сопутствовавших заболеваний (артериальная гипертензия – АГ, ишемическая болезнь сердца – ИБС, сахарный диабет – СД, онкологические заболевания), приеме и длительности применения 5-АРИ, заболеваемости COVID-19 и частоте госпитализаций по поводу COVID-19, а также проведенной пациентам вакцинации (вакцинация всем пациентам проведена с использованием вакцин Гам-КОВИД-Вак, КовиВак).
Критериями включения пациентов в исследование стали мужской пол, амбулаторное обращение в поликлинику с диагнозом «гиперплазия простаты». Критериями исключения были отсутствие информации в электронной медицинской карте относительно интересующих параметров, летальный исход в изучаемый период, наличие цистостомического дренажа.
В соответствии с критериями включения и исключения для финального анализа отобраны 1490 мужчин. Схема исследования представлена на рис. 1.
Статистическая обработка данных
Статистический анализ проведен в программах IBM SPSS Statistics, версия 26 (выпуск 26.0.0.0), и STATISTICA StatSoft, версия 12. Оценка нормальности распределения количественных переменных проводилась при помощи критерия Шапиро–Уилка (распределение всех параметров отличалось от нормального). Описательная характеристика для количественных переменных представлена в виде медианы и межквартильного интервала (IQR), для качественных переменных в виде абсолютных значений и частот.
Сравнение количественных признаков между группами проведено с использованием критерия Манна–Уитни, Значимость различий между группами по качественным признакам оценивалась на основании критерия ХИ-квадрат (χ2). Для многофакторного регрессионного анализа использован логистичесий регресс.
При проверке статистических гипотез различия считались статистически значимыми при p<0,05.
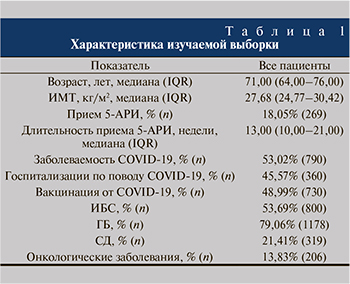
Результаты. Описательная характеристика изучаемой выборки, включившей 1490 пациентов, представлена в табл. 1. Медиана возраста мужчин составила 71 год (IQR=64–76 лет). 18,05% (269 человек) мужчин принимали 5-АРИ по поводу гиперплазии простаты, 53,02% (790) перенесли COVID-19, из них 45,57% (360) были госпитализированы из-за COVID-19. При этом 48,99% мужчин были вакцинированы от COVID-19 до заболевания.
269 мужчин изучаемой выборки (18,05%) принимали 5-АРИ по поводу гиперплазии простаты, в то время как 1221 не принимал препаратов данной группы. Сравнение показателей в двух группах пациентов (принимвших и не принимавших 5-АРИ) показано в табл. 2. Установлено, что пациенты, принимавшие 5-АРИ, оказались старше: медиана возраста составила 72 года (для не принимавших 5-АРИ 70 лет, р<0,001). При этом мужчины, принимавшие 5-АРИ, чаще вакцинировались, реже болели COVID-19 и реже госпитализировались по этому поводу.
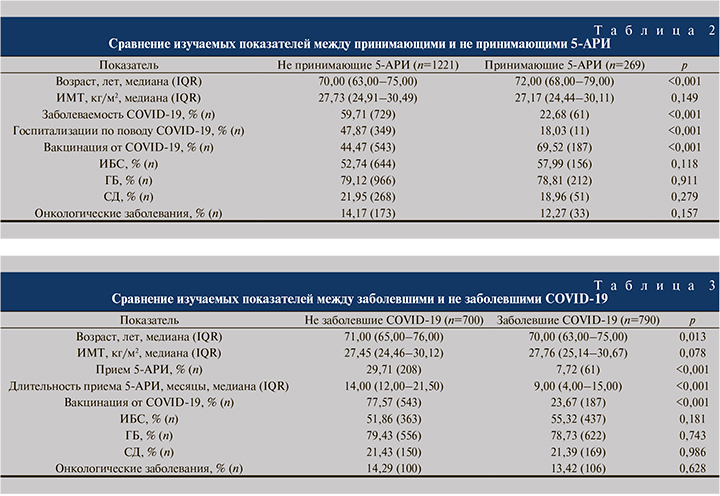
В сформированной выборке из 1490 пациентов проведен сравнительный анализ изучаемых параметров между заболевшими и не заболевшими COVID-19 (табл. 3). Показано, что не заболевшие пациенты оказались старше, чаще и дольше принимали 5-АРИ и чаще вакцинировались от COVID-19.
Графическое представление частоты и длительности приема 5-АРИ среди заболевших и не заболевших COVID-19 пациентов приведено на рис. 2.

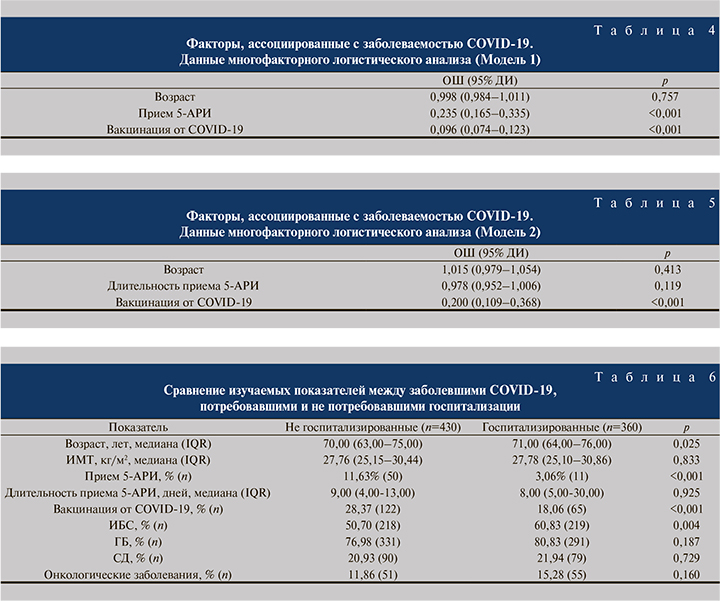
На основании проведенного выше анализа построена модель для риска заболеваемости COVID-19, включившая факторы, значимо отличавшиеся между группами заболевших и не заболевших COVID-19. Результаты представлены в табл. 4. Вакцинация от COVID-19 и прием 5-АРИ ассоциировались со снижением заболеваемости CОVID-19. Установлено, что у мужчин с ГПЖ шансы заболеть COVID-19 при приеме 5-АРИ были меньше на 76,5% (ОШ=0,235; 95% ДИ: 0,165–0,335; p<0,001). Мощным протективным фактором в нашей когорте оказалась вакцинация, шанс не заболеть у вакцинированных возрастал на 90,4% (ОШ=0,096; 95% ДИ: 0,076–0,123; p<0,001).
При замене в модели фактора «прием 5-АРИ» на «длительность приема 5-АРИ» показано, что только вакцинация от COVID-19 остается значимым фактором, ассоциированным со снижением вероятности инфицирования вирусом (табл. 5).
На следующем этапе анализа проводилась оценка влияния исследуемых факторов на тяжесть течения COVID-19, оцененную путем необходимости госпитализации пациентов. Результаты сравнения госпитализированных и не госпитализированных пациентов представлены в табл. 6. Показано, что госпитализированные с COVID-19 пациенты были старше (p=0,025), чем не госпитализированные, и чаще имели сопутствовавшую ИБС (p=0,004). При этом последние чаще принимали 5-АРИ, однако длительность приема 5-АРИ не различалась в двух исследуемых группах. Дополнительно показано, что пациенты, перенесшие COVID-19 в амбулаторных условиях, чаще были вакцинированы по сравнению с пациентами, которым потребовалась госпитализация (p<0,001).
Графическое представление частоты и длительности приема 5-АРИ среди госпитализированных и не госпитализированных с COVID-19 пациентов приведено на рис. 3.
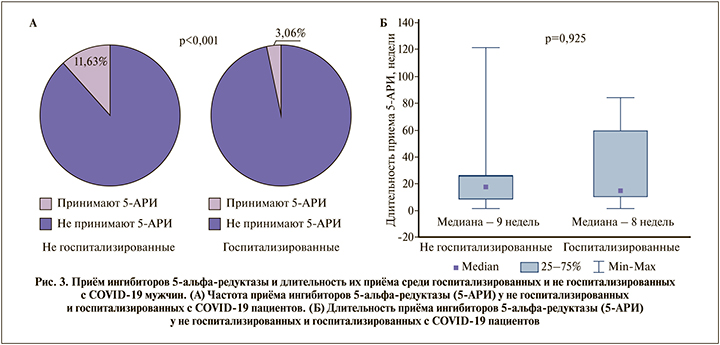
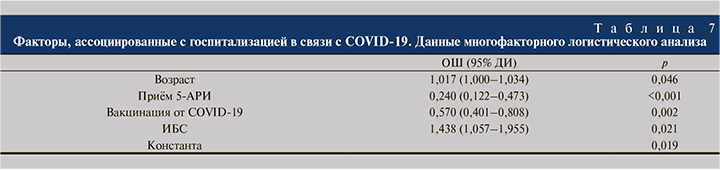
На основании проведенного анализа построена модель, включившая факторы, значимо отличавшиеся между госпитализированными и не госпитализированными по поводу COVID-19 пациентами. Результаты представлены в табл. 6. Прием 5-АРИ и вакцинация от COVID-19 ассоциировались с меньшими шансами госпитализаций независимо друг от друга. Так, при приеме 5-АРИ вероятность госпитализации снижалась на 76% (ОШ=0,240; 95% ДИ: 0,122-0,473; p<0,001). Аналогичным образом и вакцинация ассоциируется с меньшими шансами госпитализации на 43% (ОШ=0,570; 95% ДИ: 0,401–0,808; p=0,002). Факторы, ассоциированные с большим риском госпитализации в связи с тяжелым течением CОVID-19: наличие сопутствующей ИБС (+43,8%, р=0,019) и больший возраст (+1,7% при увеличение возраста на год, р=0,046).
Обсуждение результатов. Ранее мы установили, что не сниженный уровень Т ассоциируется с меньшими сроками госпитализации пациентов COVID-19 [15]. Кроме того, показано, что антагонист минералокортикоидных рецепторов, спиронолактон, обладающий также антиандрогенным действием, оказывает протективное влияние на характер течения развившейся новой коронавирусной инфекции [16]. Целью настоящего исследования было изучение заболеваемости и тяжести течения COVID-19 в зависимости от приема антиандрогенной терапии. В качестве изучаемых препаратов нами выбраны 5-АРИ. Препараты группы 5-АРИ значительно снижают сывороточную концентрацию ДГТ более чем на 70% уже с первых дней применения, не влияя при этом на сывороточную концентрацию Т [17], а по некоторым данным, даже немного повышая ее [12,13]. Здесь важно акцентировать внимание, что повышенный уровень тестостерона сопровождается ростом уровня интерлейкина 10, способствующего снижению уровня TNF-α [18, 19].
Таким образом, механизм действия 5-АРИ предполагает возможность их защитного эффекта в отношении частоты заболеваемости COVID-19 и частоты госпитализаций:
- за счет как снижения уровня ДГТ, усиливающего возможности проникновения вируса SARS-CoV-2 в клетки [20],
- так и компенсаторного увеличения содержания Т в плазме, который обладает протективными эффектами в виде снижения активации провоспалительных цитокинов, уменьшения риска развития ОРДС и тромбозов и тромбоэмболий [15].
Результаты проведенного исследования показали, что применение 5-АРИ у мужчин с ГПЖ ассоциированы со снижением риска заболевания COVID-19 на 76,5%, уступив по протективному эффекту лишь факту наличия вакцинации против новой коронавирусной инфекции, ассоциированной со снижением риска заболевания COVID-19 на 90,4% (р<0,001).
В нашем исследовании впервые изучено влияние длительности приема 5-АРИ на заболеваемость COVID-19 и частоту госпитализации по этому поводу. Длительность лечения 5-АРИ оказалась большей в группе больных, избежавших COVID-19 (14 недель против 9, р<0,001), но в многофакторном анализе она теряла статистически значимое влияние на шансы заболеть новой коронавирусной инфекцией. Частично это может быть связано с ретроспективным анализом данных [21]. Другое возможное объяснение этого факта дают публикации 1992 г., когда было показано, что концентрация ДГТ снижается до минимальных значений уже в первые дни приема препарата и остается на данном уровне в течение всего приема, при этом не влияя на концентрацию Т [22].
Полученные результаты затрагивают актуальную область и эффективность антиандрогенной терапии при COVID-19 остается дискутабельной. Известно, что 5-АРИ блокируют фермент 5-альфа-редуктазу, присутствующую в том числе в респираторном эпителии для поддержания равновесия андрогенов и тем самым слоя сурфактанта [23]. Кроме этого 5-АРИ могут нарушать метаболизм андрогенов в легких, препятствуя регенерации респираторного эпителия и, соответственно, повышению вероятности развития и усугубления острого респираторного дистресс-синдрома, характерного и для COVID-19 [24]. Дальнейшее изучение данного вопроса в связи с наличием подобных опасений заключалось в проведении обсервационных исследований, сравнивающих заболеваемость и тяжесть течения COVID-19 среди пациентов, принимающих и не принимающих 5-АРИ по поводу сопутствующих заболеваний (чаще всего андрогенной алопеции и гиперплазии простаты).
В январе 2022 г. опубликовано исследование, изучившее взаимосвязь приема 5-АРИ с заболеваемостью COVID-19 двух сопоставимых по клиническим характеристикам когортаов пациентов: принимавших (n=944) и не принимааших 5-АРИ (n=944). В ходе анализа показано, что риск инфицирования SARS-Cov-2 у принимавших 5-АРИ пациентов был в 1,23 раза ниже, чем у не принимавших АДТ: число заболевших в данных группах составило 42,3 и 47,2% соответственно (p=0,026) [25]. Полученные данные привели исследователей к выводу о защитном влиянии данной группы препаратов в отношении заболеваемости COVID-19, что было подтверждено и в нашем исследовании. Риск инфицирования SARS-Cov-2 при введении поправки на возраст и вакцинацию при приеме 5-АРИ был на 76,5% меньше. 29,7% не заболевших принимали 5-АРИ, в то время как среди заболевших данный показатель был существенно ниже и составил 7,7% (p<0,001).
В ретроспективном анализе популяционной когорты пациентов, проведенном с использованием данных британского биобанка (n≈397,000), выполнен скрининг лекарственных препаратов и вакцин (n=819) на предмет их связи с COVID-19. Показана ассоциация 5-АРИ наряду с рядом других препаратов с меньшим риском заболеваемости и более тяжелого течения COVID-19 [26].
В исследовании, выполненном в Ломбардии, обследованы 943 пациента, госпитализированных с подтвержденным диагнозом COVID-19, и сопоставимые по возрасту мужчины, находившиеся на амбулаторном лечении. Установлено, что госпитализированные мужчины старше 55 лет принимали 5-АРИ значительно реже, чем не госпитализированные (5,57 и 8,14% соответственно; p=0,008). Среди мужчин старше 65 лет диспропорция в приеме 5-АРИ между госпитализированными и не госпитализированными пациентами увеличивается: 7,14 и 12,31% соответственно; (р=0,0001). На основании полученных результатов исследователями сделан вывод: мужчины, принимавшие 5-АРИ, могут быть менее уязвимы к тяжелой форме COVID-19 и, соответственно, для них характерна меньшая частота госпитализаций, что оправдывает использование препаратов данной группы в качестве профилактики [27]. Аналогичные результаты получены и в представляемом исследовании. 3,06% госпитализированных с COVID-19 пациентов принимали 5-АРИ, в то время как среди мужчин с COVID-19, находившихся на амбулаторном лечении, данный показатель оказался значительно больше и составил 11,63% (p<0,001).
По результатам ретроспективного когортного исследования, проведенного в Испании в 2021 г., среди мужчин с облысением, принимавших 5-АРИ, частота возникновения и выраженность клинических проявлений при COVID-19 (аносмия, потеря вкусовых ощущений, головная боль, сухой кашель, лихорадка, судороги, слабость, боли в спине и диарея) была статистически значимо ниже, чем среди пациентов, не принимавших 5-АРИ [28]. На основании полученных результатов проведено слепое рандомизированное проспективное исследование, где пациентам с подтвержденным COVID-19 назначался препарат группы 5-АРИ дутастерид (n=64) или плацебо (n=66). Исчезновение симптомов, таких как усталость, аносмия и агевзия, происходило в 2 раза быстрее среди пациентов, принимавших дутастерид. Время до наступления полной ремиссии COVID-19 составило 9 дней для пациентов, принимавших дутастерид, и 15,6 дня для контрольной группы, что указывало на протективный эффект данной группы препаратов в отношении тяжести симптомов COVID-19 [29]. В нашем исследовании препараты этого класса снижали частоту госпитализаций по поводу тяжелого течения новой коронавирусной инфекции.
При этом следует учитывать, что показания к назначению ингибиторов 5-альфа-редуктазы весьма ограниченны: в первую очередь это доброкачественная гиперплазия предстательной железы и в некоторых случаях андрогенная алопеция. Трудности в назначении 5-АРИ в качестве стратегии лечения и профилактики COVID-19 связаны и с возможными побочными эффектами, значительно ухудшающими качество жизни мужчин: депрессия, снижение либидо, эректильная дисфункция. Тем не менее распространенность данных побочных эффектов не превышала 16% [30]. В последние годы активно рассматривается вопрос об онкологической безопасности 5-АРИ. Несмотря на то что большинство исследований не выявил ассоциации приема 5-АРИ с риском развития рака простаты, однако сообщалось о более частом выявлении рака простаты high grade. При этом использование 5-АРИ не влияло на выживаемость пациентов с раком предстательной железы [30]. Поэтому при назначении данной группы препаратов в качестве возможной стратегии профилактики и лечения COVID-19 следует учитывать имеющиеся на сегодняшний день показания и возможные побочные эффекты 5-АРИ.
Впервые в настоящем исследовании показано, что длительность приема 5-АРИ не влияла ни на риск заболеваемости COVID-19, ни на частоту госпитализации по поводу развившейся новой коонавирусной инфекции. Возможны два объяснения:
- ретроспективный характер исследования, не позволяющий точно вычислять реальную длительность приема назначенных 5-АРИ пациентами [21];
- быстрый эффект от применения 5-АРИ, при котором концентрация ДГТ снижается до минимальных значений уже в первые дни приема препарата и остается на данном уровне в течение длительного времени, при этом не влияя или даже повышая концентрацию Т [22].
Ограничением нашего исследования является ретроспективный характер, в связи с которым не известны все причины назначения и неназначения АРИ-5, проведения и непроведения вакцинации. Также не было возможности провести оценку: отличалось ли время наблюдения пациентов, получавших и не получавших 5-АРИ, при этом разница в сроках наблюдения могла влиять на полученный результат.
Заключение. Принм 5-АРИ наряду с проведением вакцинации для пациентов с гиперплазией предстательной железы является протективным фактором в отношении риска заболеваемости новой коронавирусной инфекцией и тяжести течения COVID-19, требовавшей госпитального лечения. Целью будущих проспективных рандомизированных клинических исследований должно стать изучение терапии 5-АРИ в качестве возможной стратегии профилактики и лечения COVID-19 у четко подобранной группы пациентов с учетом показаний и возможных побочных эффектов данной группы препаратов.