Анатомически органы малого таза находятся в тесном контакте друг с другом. В урологии и колопроктологии имеет значение близость прямой кишки и мочеполовых органов, так как это может приводить к общим проявлениям заболеваний и/или имитации симптомов со стороны непораженной области из-за близости с патологическим очагом другой системы, что затрудняет диагностический процесс. Данные особенности должны учитываться соответствующими специалистами. Отсутствие «широкого» взгляда на возможные проблемы со стороны органов малого таза может приводить к диагностическим ошибкам, а следовательно, и к неправильному выбору лечебной тактики.
Цель настоящего обзора – охарактеризовать возможные урологические проявления заболеваний прямой кишки при вовлечении мочеполовой системы, а также симптомы урологических заболеваний, вовлекающих дистальные отделы кишечника.
Простатит. Широкий спектр рекомендуемых методов лечения простатита указывает на то, как мало известно о его этиопатогенезе, методах диагностики и лечения. Тем не менее простатит остается наиболее частой причиной амбулаторных посещений урологов мужчинами в возрасте до 50 лет. Согласно эпидемиологическим исследованиям 11–16% мужчин имеют диагноз простатита в текущий момент либо в анамнезе [1–3], а к 85 годам вероятность установления диагноза острого или хронического простатита составляет 26% [4]. Данные Национального центра статистики здравоохранения США показывают, что визи-
ты по поводу простатита происходят чаще, чем по поводу гиперплазии или рака предстательной железы [3].
Выделяют четыре категории простатита [2]:
I. Острый бактериальный простатит.
II. Хронический бактериальный простатит (хроническая инфекция предстательной железы характеризуется рецидивирующими инфекциями мочевыводящих путей [ИМП]).
III. Хронический простатит/синдром хронической тазовой боли:
IIIA. Воспалительный (значительное количество лейкоцитов, без уропатогенных бактерий, культивируемых стандартными методами в секрете предстательной железы, постмассажной порции мочи или эякуляте).
IIIB. Невоспалительный (симптомы дискомфорта или боли в области таза 3 мес. и более в отсутствие лейкоцитов и уропатогенных бактерий в секрете предстательной железы, постмассажной порции мочи или эякуляте).
IV. Асимптомный воспалительный простатит (повышение содержания лейкоцитов в секрете предстательной железы, постмассажной порции мочи, эякуляте или ткани предстательной железы при гистологическом исследовании без симптомов простатита).
Простатит I типа (острый бактериальный простатит) относительно легко диагностируется на основании положительных культуральных исследований секрета предстательной железы; на его долю приходится около 5% пациентов с простатитом. Хронический простатит встречается гораздо чаще, но его труднее диагностировать и лечить. Хронический бактериальный простатит встречается редко, составляя примерно 5% больных простатитом. Более 90% случаев простатита — это хронический абактериальный простатит [4, 5].
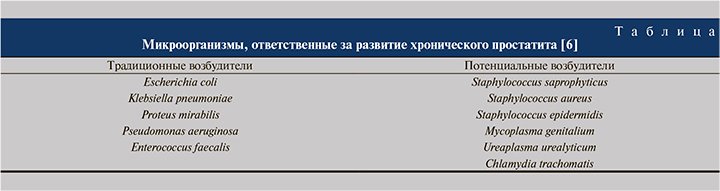
Острый простатит — это инфекционное воспалительное заболевание предстательной железы. Хроническим называют инфекционный воспалительный процесс в предстательной железе длительностью более 3 мес. [4]. Наиболее частым микроорганизмом, выявляемым при остром простатите, является Escherichia coli (65–80%), в то время как Pseudomonas aeruginosa, виды Serratia, виды Klebsiella и Enterobacter aerogenes встречаются в 20–35% случаев. Микроорганизмы, ответственные за хронический бактериальный простатит, представлены в таблице [6].
Другими значимыми инфекционными агентами в развитии простатита являются вирусы (вирус простого герпеса 1-го и 2-го типов, цитомегаловирус), грибки, а также, например, Neisseria gonorrhea, которая была распространенной причиной простатита в доантибиотическую эпоху [5–7].
Диагностика. Простатит I и II категорий.
Острый простатит – тяжелое системное заболевание, клинически проявляющееся симптомами, характерными для ИМП (дизурия); простатита (боль в пояснично-крестцовой области, промежности, половом члене и иногда в прямой кишке); бактериемии (лихорадка, озноб, артралгия, миалгия, тахикардия).
Ведущими симптомами острого бактериального простатита являются острое начало, лихорадка, озноб, боль в промежности и общее недомогание. Обструктивная и ирритативная симптоматика обусловлена отеком предстательной железы и сдавлением простатического отдела мочеиспускательного канала, которая усиливается на фоне доброкачественной гиперплазии и рака предстательной железы, рака мочевого пузыря, склероза шейки мочевого пузыря, стриктуры уретры, а также при нейрогенных дисфункциях нижних мочевыводящих путей. Следует избегать массажа предстательной железы и трансуретральных манипуляций, чтобы предотвратщать распространение инфекционного процесса вплоть до развития уросепсиса [4].
Хронический бактериальный простатит (категория II) предполагает наличие в анамнезе документированных рецидивирующих ИМП. В промежутках между эпизодами обострений ИМП пациенты могут либо не иметь симптомов, либо испытывать дискомфорт и/или боль в малом тазу. При хроническом простатите простата при пальпации может быть тугоэластичной или иметь пастозную консистенцию.
Простатит IIIВ и IV категорий. Синдром хронической тазовой боли/хронический небактериальный простатит (категория IIIB) является наиболее распространенным и выявляется чаще, чем другие формы простатита. Сложность диагностики этой формы объясняется тем, что под маской хронического простатита может протекать более 20 различных заболеваний. Ведущими симптомами данного заболевания являются расстройства мочеиспускания, копулятивные нарушения и боли в области таза, при этом отмечается отсутствие признаков воспалительной реакции в моче, секрете предстательной железы и сперме.
Перечисленные симптомы часто имеют неспецифический характер. Боль преимущественно локализуется в промежности, у основания полового члена или надлобковой области.
Боль, возникающая во время или после эякуляции, является характерной, но не патогномоничной особенностью хронического простатита. Симптомы, возникающие при опорожнении мочевого пузыря, включают учащенное, слабое и прерывистое мочеиспускание, что приводит к снижению качества жизни пациентов. Тяжесть симптомов может быть оценена по специальному опроснику «Индекс шкалы симптомов хронического простатита и синдрома тазовых болей у мужчин (ХП-СХТБ)». При физикальном осмотре пальпация предстательной железы может быть болезненной с иррадиацией боли в половой член или в яички.
Этиология хронической тазовой боли сложна и мультифакторна. Вероятными причинами являются инфекции, аутоиммунные реакции, нервно-мышечные спазмы, ущемление нервных структур и т.д. Chlamydia trachomatis – основной этиологический фактор хронического небактериального простатита, при этом антитела к C. trachomatis обнаруживаются в 30% случаев [8].
C. trachomatis также была обнаружена в ректальных выделениях у 31% мужчин с гистологическими признаками простатита [9]. Однако, поскольку выявление хламидийной инфекции является сложной задачей, ее причинная роль до конца не установлена [10]. Другим важным фактором развития простатита является детрузорно-сфинктерная диссеннергия [9].
Воспалительный простатит (категория IV) – это бессимптомное заболевание, которое диагностируется путем гистологического исследования материала, полученного при резекции доброкачественной гиперплазии или биопсии предстательной железы. Пациенты, как правило, не имеют симптомов, поэтому при установлении этого диагноза лечения не требуется.
Острый бактериальный простатит помимо трансректального УЗИ требует проведения посева средней порции мочи для подтверждения диагноза. Для диагностики хронического простатита посевы средней порции мочи неубедительны, поэтому необходимо дальнейшее детальное обследование. Трехстаканная проба мочи позволяет определить, являются ли источником инфекции уретра, мочевой пузырь или предстательная железа (рис. 1) [6].
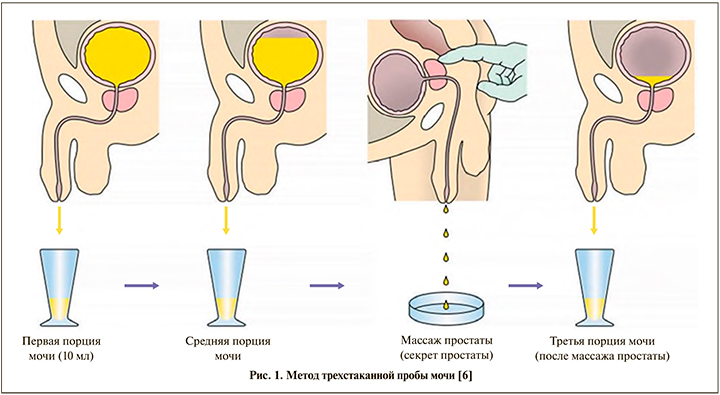
Начальные 10 мл опорожненной мочи представляют собой образец мочи из уретры. Средняя порция мочи представляет собой мочу из мочевого пузыря. Третья порция мочи представляет собой первые 10 мл мочи, выделенной после массажа предстательной железы, ее также называют секретом простаты.
Наличие уропатогенных бактерий в секрете предстательной железы или постмассажной порции мочи позволяет установить диагноз хронического бактериального простатита, если эти бактерии отсутствуют (или их концентрация в 10 раз меньше) в уретральной и мочепузырной порциях. Выделение непатогенных микроорганизмов из секрета простаты и/или в постмассажной порции мочи и наличие более 10 лейкоцитов в поле зрения свидетельствуют о воспалительном синдроме хронической тазовой боли (категория IIIA).
Хронический бактериальный простатит может быть установлен при выявлении десятикратного увеличения количества бактерий в третьей порции мочи по сравнению с ее первой и средней порциями. Отсутствие изменений во всех порциях мочи, а также стерильность исследуемого материала позволяют устанавливать диагноз невоспалительного синдрома хронической тазовой боли (категория IIIB) [9].
Энтеровезикальный свищ. Свищ – это эпителизированный тракт-сообщение между двумя полыми органами или полым органом и поверхностью тела. Свищи образуются, когда пролиферативные процессы, травма или воспаление, возникшие в одном полом органе, распространяются за его границы и вовлекают другой полый орган или поверхность кожи и слизистых. Мочеполовые свищи разнообразны по клинической картине и этиологии, могут вовлекать желудочно-кишечный тракт, сосудистую, лимфатическую системы и кожу [11].
Мочекаменная болезнь, ятрогенная травма, дивертикулит, лучевая терапия и туберкулез являются одними из основных причин уретро-кишечных свищей [11, 12]. Пациенты с уретеро-кишечными свищами могут предъявлять разнообразные жалобы, включая боль в животе, кровь в моче, рецидивирующие ИМП, фекалурию и диарею. Самым ярким и патогномоничным симптомом является появление газа и/или кала в мочевыводящих путях. В установлении диагноза помогают визуализирующие исследования, такие как внутривенная урография, цистография, цистоскопия, ретроградная пиелография и компьютерная томография с контрастированием (КТ) или магнитно-резонансная томография [12].
Кишечные фистулы мочевого пузыря (коловезикальные, толстокишечно-пузырные) чаще всего возникают при осложненном дивертикулите, новообразованиях желудочно-кишечного тракта или мочевыводящей системы, воспалительных заболеваниях кишечника [13], а также после лучевой терапии и операций в области органов малого таза. Появление указанных свищей в первую очередь связано с анатомической близостью дистальных отделов кишечной трубки и мочевыводящих путей, подвижностью сигмовидной кишки. Коловезикальные фистулы как осложнение дивертикулярной болезни составляют 65% всех кишечных фистул [14]. Причиной развития патологического соустья между кишкой и мочевым пузырем также может быть злокачественное поражение толстой кишки или мочевого пузыря. Ректовезикальные фистулы почти всегда возникают из-за злокачественных новообразований или травм одного из смежных органов — мочевого пузыря или прямой кишки [13].
Клинически колоили ректовезикальная фистула проявляется рецидивирующим циститом, пневматурией, фекалурией, лихорадкой и болью в животе. Компьютерная томография является основным неинвазивным методом визуализации при подозрении на заболевание; типичными диагностическими маркерами являются внутрипузырный воздух и очаговое утолщение стенки мочевого пузыря в области прилежания к кишечной стенке. Тем не менее, данное исследование не всегда может продемонстрировать фистулу из-за малых размеров последней или ее «маскировки» в массивном воспалительном процессе (рис. 2А) [12]. Рентгенография с введением водорастворимого контраста в просвет кишки (проктография) или мочевой пузырь (цистография) выявляет 35% всех фистул, а цистограмма в момент опорожнения мочевого пузыря может визуализировать фистулу в 10–40% случаев (рис. 2Б) [12, 15, 16].
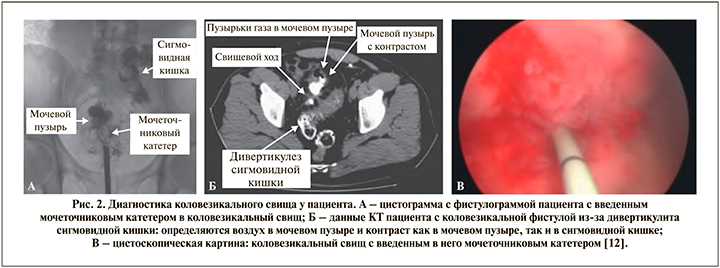
Цистоскопия может выявлять свищевое отверстие (рис. 2В) [12]. Внутривенное введение метиленового синего или индигокармина помогает идентифицировать повреждение. Дополнительно может быть использована ректосигмоскопия, которая позволяет визуализировать свищевое отверстие в 55% случаев [17, 18]. Другим исторически интересным, но простым диагностическим тестом является пероральный прием семян мака, обнаружение которых в моче указывает на энтеровезикальную фистулу [19].
Большинству пациентов требуется хирургическое вмешательство. В зависимости от первичного процесса, приведшего к образованию свища, и активности перифокального воспалительного процесса проводят различные по объему резекции пораженного сегмента толстой кишки с формированием первичных анастомозов или выполнением обструктивных резекций по Гартману.
Повреждение мочеточника при колоректальной хирургии. Оперативные вмешательства на органах малого таза потенциально опасны в первую очередь непреднамеренной травмой мочеточника. Как правило, мочеточники вовлекаются в патологический процесс при массивных местнораспространенных и рецидивных опухолях прямой кишки или воспалительных изменениях сигмовидной кишки (например, при дивертикулите, болезни Крона и т.д.). Гинекологические вмешательства сопряжены с относительно высоким риском урологических осложнений, в первую очередь из-за анатомической близости маточных сосудов и дистальных отделов мочеточников, а также вследствие вовлечения элементов мочевыделительной системы в патологический эндометриоидный инфильтрат. Частота ятрогенных повреждений мочеточника варьируется от 1 до 10% [20].
При ятрогенном повреждении типичными травмами являются прошивание мочеточников, раздавливание зажимами, полное пересечение или краевая травма, деваскуляризация мочеточника, например при мобилизации последнего из опухолевого или воспалительного инфильтрата.
Выявление травмы мочеточника во время операции имеет первостепенное значение. Однако только 20–60% повреждений мочеточника распознаются во время операции [20]. Пациентам требуется в среднем две восстановительные процедуры для реконструкции мочеточника при обнаружении повреждения в послеоперационном периоде по сравнению с одной процедурой при своевременном обнаружении травмы во время операции. Кроме того, быстрое распознавание повреждения мочеточника с немедленным его восстановлением приводит к меньшему числу осложнений или нарушений функции почек [20].
Если повреждение мочеточника не распознается во время операции, то в раннем послеоперационном периоде могут наблюдаться такие симптомы, как анурия, боль в области мочеточника, макрогематурия, гидронефроз с лихорадкой или без нее, выделение мочи через брюшные дренажи и т.д. Компьютерная томография с контрастом брюшной полости позволяет выявлять затеки мочи в забрюшинное пространство или брюшную полость. Внутривенная урография, совмещенная с ретроградной урографией, документируют степень стриктуры и расстояние между травмой и мочевым пузырем. В сочетании с цистографией они также исключают или подтверждают мочеточниковую или пузырную фистулу [20, 21].
Профилактика повреждений мочеточника. Переоценить важность точного знания топографической анатомии и возможных вариаций расположения органов малого таза невозможно. Основным условием безопасности хирургических вмешательств является точное следование принципам эмбрионально-ориентированной мобилизации структур малого таза без нарушения целостности соседних компартментов. Однако воспалительные и местнораспространенные опухолевые процессы могут существенно изменять локализацию тазовых структур, стирать границы между мочеточниками и смежными органами и/или вовлекать мочеточники в неразделимые опухолевые конгломераты. При возникновении необходимости в идентификации мочеточников существует правило: поиск необходимо начинать проксимальнее зоны хирургического интереса и затем визуализировать мочеточник на всем его протяжении до места впадения в мочевой пузырь. При затруднении идентификации мочеточников интраоперационно ретроградно устанавливают мочеточниковые стенты, помогающие пальпаторно и визуально (в случае установки светящихся стентов) определить ход органа. Установка стентов не снижает риска повреждения мочеточников, однако многократно повышает вероятность своевременного выявления повреждения [21].
Повреждения мочевого пузыря. Ятрогенные повреждения мочевого пузыря во время операций на толстой и прямой кишке встречаются редко, с частотой примерно 0,06% [22]. Повреждение мочевого пузыря может быть распознано интраоперационно при обнаружении мочевого катетера в хирургическом поле или появлении мочи из нераспознанного дефекта мочевого пузыря. Иногда травма мочевого пузыря остается нераспознанной, если размер дефекта невелик. В такой ситуации полностенное ранение мочевого пузыря может быть подтверждено появлением красителя в операционном поле после введения в мочевой пузырь раствора метиленового синего через катетер. Нагнетание красителя в мочевой пузырь используют также для идентификации границ мочевого пузыря во избежание его травмы. К счастью, мочевой пузырь обладает выраженными регенераторными возможностями.
Непреднамеренное повреждение практически всегда самостоятельно заживает, если мочевой пузырь своевременно дренировать трансуретральным или надлобковым катетером и герметично ушить стенку мочевого пузыря. Метод ушивания не имеет большого значения: могут быть использованы узловые или непрерывные швы, двухрядные или однорядные швы, при этом крайне важно использовать только рассасывающийся шовный материал во избежание камнеобразования.
Повреждения уретры. Этиология. Непреднамеренное повреждение уретры осложняет примерно 0,04% операций на толстой и прямой кишке и от 0,7 до 2% всех резекционных вмешательств на органах малого таза [23, 24]. При колоректальных вмешательствах это чаще происходит во время брюшно-промежностной экстирпации прямой кишки и низких передних резекциях прямой кишки. В случае подозрения на травму уретры внутривенно вводят индигокармин или метиленовый синий, что сопровождается выделением окрашенной мочи из места травмы. Послеоперационное обнаружение повреждения уретры обычно происходит после того, как моча начинает вытекать из раны или через тазовый дренаж. Диагноз подтверждается анализом жидкости на содержание мочевины и креатинина. Профилактика и восстановление. Необходимо проявлять большую осторожность при выполнении резекций прямой кишки и при резекционных вмешательствах в аноректальной области. Риск травмы многократно повышается при местнораспространенных опухолях прямой кишки, наличии паратуморозных абсцессов, при болезни Крона, осложненной свищами аноректальной зоны или образованием воспалительных инфильтратов и абсцессов после лучевой терапии. Наиболее важным аспектом является своевременное обнаружение травмы. Это может оказаться очень сложной задачей, особенно при вовлечении основания мочевого пузыря или простатической части уретры. При таком повреждении восстановление целостности уретры, возможно, придется дополнить оментопластикой с надлобковым дренированием предпузырного пространства.
При позднем обнаружении уже сформированного ректоуретрального свища требуется содружественное участие уролога и колопроктолога, досконально знающих анатомию малого таза и владеющих различными вариантами реконструктивных операций. Большинство ректоуретральных свищей возникает после операций по поводу злокачественных новообразований предстательной железы, но может возникать и после операций по поводу доброкачественных заболеваний предстательной железы. Лишь в редких случаях они являются результатом колоректальных операций, как правило, при распространенном злокачественном новообразовании прямой кишки, после лучевой терапии или болезни Крона. Иссечение этих свищей может быть выполнено с помощью трансвезикального или трансанального доступа. В качестве альтернативы можно выбрать трансперинеальный путь или, как в случае операции Мэйсона, парасакральный разрез с рассечением задней полуокружности прямой кишки. Резекции прямой кишки с рукавным колоанальным анастомозом сегодня выполняются редко. Надлобковая декомпрессия хирургического поля обязательна после операции [25].
Таким образом, важно подчеркнуть краеугольные моменты коррекции возможных урологических осложнений тазовой хирургии. Во-первых, основные усилия хирурга должны быть сосредоточены на предотвращении непреднамеренных травм мочевой системы. Профилактические мероприятия включают два основных пособия: предварительное стентирование мочеточников для упрощения их визуализации и интраоперационное наполнение мочевого пузыря для облегчения визуализации границ мочевого пузыря. Диагностика состоявшихся травм значительно облегчается внутрипузырным или внутривенным введением красителя. В лечении травм полых органов мочевой системы первоочередной задачей является «осушение» зоны повреждения с помощью формирования нефростом, эпицистостом, наружной катетеризации чашечно-лоханочной системы почек. При травмах, вовлекающих помимо мочевой системы просвет прямой кишки, может понадобиться формирование временной колостомы с той же целью – «осушения» зоны ранения от каловой струи. При состоявшейся травме мочеточников оптимальным способом коррекции является одномоментное формирование неоуретеро-цистоанастомоза.
Глубокое знание анатомии мочеполовой системы, а также стратегий выявления и устранения потенциальных повреждений имеет первостепенное значение. Особое внимание необходимо уделять при операциях в узких пространствах таза, поскольку именно здесь эти структуры подвергаются наибольшему риску. Факторы, влияющие на пациента, включая предшествующую операцию на органах малого таза, облучение, воспалительные заболевания кишечника, инфекционные процессы и аномалии мочеполовой системы, – все это увеличивает риск травм.