Введение. Варикоцеле (В) – распространенное нарушение половых органов, которое может быть связано с мужским бесплодием и гипогонадизмом [1]. По данным ВОЗ конца прошлого века, его распространенность оценивали примерно в 25% у мужчин с аномальным анализом спермы при 12% в нормальной мужской популяции [2]. По последним данным, В диагностируется у 35–40% мужчин с бесплодием [1], при этом среди мужчин с первичным бесплодием оценивается в 35–44%, с вторичным – в 45–81% [3, 4]. Принято считать, что повышенная температура мошонки, гипоксия и рефлюкс токсических метаболитов могут вызывать дисфункцию яичек и бесплодие из-за увеличения оксидативного стресса (ОС) и повреждения ДНК [1, 4–8]. При этом ухудшение параметров спермы связано с более высокой степенью В и возрастом [9, 10].
Однако имеющиеся данные оставляют много неясных вопросов. По-прежнему точная связь между снижением мужской фертильности и В не очевидна: более 2/3 мужчин с В фертильны [11–14]. Варикоцелэктомия далеко не всегда приводит к улучшению качества спермы и восстановлению фертильности: улучшение спермограммы после операции обычно имеет место в 60-80% случаев, беременности в естественном цикле наступают у 30–45% пар [6, 15–19]. Улучшение целостности ДНК спермы после варикоцелэктомии составляет в среднем всего -3,4% (95% ДИ от -2,65 до -4,09) [20].
Поэтому по-прежнему актуальны многие вопросы, связывающие В и мужскую фертильность. Насколько на фоне В снижается качество спермы и повышается риск бесплодия? Какова роль дополнительных факторов? Кому действительно необходима варикоцелэктомия?
В этой статье мы представим данные по эпидемиологии В у пациентов из бесплодных пар, охарактеризуем взаимосвязь варикоцеле с показателями спермы и реальной фертильностью.
Цель исследования: оценить количественную взаимосвязь между В и репродуктивной функцией на большой выборке.
Тип исследования: многоцентровое поперечное и случай–контроль.
Материалы и методы. Ретроспективно проанализированы электронные истории болезни 3632 мужчин в возрасте от 18 до 45 лет, обратившихся в клиники уроандрологического профиля Москвы, где работают авторы, по поводу отсутствия желанной беременности в браке более 1 года. Пациенты прошли комплексное клинико-лабораторное обследование в соответствии с рекомендациями ВОЗ [3, 21, 22]. Наличие и степень выраженности В оценивали в соответствии с рекомендациями WHO [3] и EAU [1]. Аналогично были обследованы 276 фертильных мужчин, обратившихся по различным поводам (диспансеризация, сексуальные проблемы, симптомы нижних мочевых путей и др.), от которых в течение 3 мес., предшествовавших обращению, наступила спонтанная беременность без какого-либо специфического лечения. Эти мужчины сформировали контрольную группу; исход наступившей беременности при этом не учитывался.
На первом этапе провели корреляционный анализ взаимосвязи наличия и степени В с показателями спермограммы (n=3908): объемом, концентрацией, подвижностью различных категорий, морфологией, расчетным числом прогрессивно подвижных сперматозоидов в эякуляте (ЧППСЭ: объем х концентрация х доля прогрессивно подвижных сперматозоидов), фрагментацией ДНК и др., а также данными клинического обследования. Критерии включения: возраст мужчины – 18–45 лет, наличие или отсутствие и степень В по данным физикального обследования, результаты исследования спермы по критериям ВОЗ [21], анамнестические данные о продолжительности бесплодия, наличии/отсутствии беременности от мужчины в прошлом, в т.ч. в течение последних 3 мес., регулярная половая жизнь без контрацепции не реже 1 раза/нед. Критерии исключения: отсутствие необходимых клинико-лабораторных данных, пациенты с концентрацией сперматозоидов менее 1 млн/мл, как имеющие высокий риск генетических аномалий [1, 23].
На втором этапе сравнили распространенность В различной степени в группах: 1) фертильных мужчин (n=276), 2) пациентов из пар с первичным бесплодием (n=2284) и 3) вторичным бесплодием (n=1348), а также в подгруппах с олигоастенотератозооспермией (ОАТ-синдром). Критерии включения: в группу 1 – установленный факт наступившей беременности в течение последних 3 мес. (с учетом продолжительности цикла сперматогенеза); в группу 2 – отсутствие беременностей у женщин-партнерш как в браке, так и до брака; в группу 3 – известен факт беременностей у партнерш более 1 года назад независимо от их исхода; для подгрупп с ОАТ-синдромом – соответствие данному диагнозу по критериям ВОЗ [21]. Критерии исключения: отсутствие необходимых клинико-лабораторных данных, пациенты с концентрацией сперматозоидов менее 1 млн/мл, нерегулярная половая жизнь без контрацепции реже 1 раза/нед., тяжелые соматические и психические заболевания. Группы были сопоставимыми, статистические различия по перечню учитываемых показателей, кроме дискриминантного – факта и времени наступления беременности, между группами отсутствовали.
Используемые методы исследования: общеклиническое обследование, оценка качества эякулята в соответствии с требованиями ВОЗ [21], определение антиспермальных антител (АСАТ) методом MAR%IgG и IgA (SpermMar Kit, FertiPro, Belgium), определение фрагментации ДНК сперматозоидов методом дисперсии хроматина в агарозном геле [24].
Статистические методы исследования с применением «Microsoft Excel» и «Statistica» (StatSoft, США). Анализ соответствия вида распределения признака закону нормального распределения проводили по критерию Шапиро–Уилка (Shapiro–Wilk/S-W). Средние значения по группам представляли в виде M±SD, медианы, 25–75% процентилей, диапазона «невыпадающих значений». Значимость различий между группами проверяли с помощью критериев Стьюдента (t), Манна–Уитни (M-W), знаков (Z), ХИ-квадрат (χ); для анализа корреляционной зависимости применяли непараметрические критерии Спирмена (R) и Гама (γ); различия считали значимыми при p<0,05.

Все мужчины дали информированное согласие на использование данных их обследования в научных целях.
Результаты. Возраст фертильных мужчин, включенных в исследование, – 32,1±5,5 лет; пациентов из бесплодных пар, включенных в исследование, – 33,1±5,7 года (p>0,05); в отдельных группах и подгруппах – в табл. 2.
Результаты корреляционного анализа между степенью В и показателями качества эякулята для разных групп и подгрупп представлены в табл. 1. Во всех группах и подгруппах существует значимая отрицательная взаимосвязь между степенью В и концентрацией сперматозоидов: -0,15 (p<0,05) для фертильных, -0,11 для всей выборки из бесплодных пар (p<0,001), в т.ч. -0,10 при ОАТ-синдроме (p=0,05). Процент прогрессивно подвижных и морфологически нормальных сперматозоидов, объем и другие показатели эякулята не зависят от степени В ни в одной из оцениваемых групп (p>0,05). ЧППСЭ снижается пропорционально степени В, но сила связи меньше, чем для концентрации, и значима только для всей выборки мужчин из бесплодных пар (-0,08; p<0,001). Аналогично взаимосвязь между фрагментацией ДНК сперматозоидов и степенью В значима только для всей выборки мужчин из бесплодных пар (0,11; p<0,001), но не для фертильных и с ОАТ-синдромом (p>0,05).
Анализ распространенности В показал (табл. 2), что у мужчин из бесплодных пар (n=3632) В диагностировано в 1073 (29,5%) случаях: 783 (21,6%) – первая степень, 250 (6,9%) – вторая, 40 (1,1%) – третья. При первичном бесплодии (табл. 2) 28,1% случаев диагностированного В, в т.ч. первая степень – 20,2%, вторая – 6,9%, третья – 1,0%. При вторичном бесплодии (n=1348) В встречалось незначительно чаще, чем при первичном, – 31,6% (ОШ=1,13; p<0,05), в т.ч. первая степень – 23,5% (ОШ=1,16; p<0,05), вторая – 6,8% (p>0,05), третья – 1,3% (p>0,05).
В подгруппах бесплодных мужчин с ОАТ-синдромом (рис. 1) В при первичном бесплодии (n=322) имело место: первая степень – у 20,8%, вторая – у 9,3%, третья – у 1,2% пациентов. При вторичном бесплодии с ОАТ-синдромом (n=125): соответственно – 15,2%, 16,0 и 3,2% случаев. Различия между данными подгруппами не существенны (p>0,05). Мужчины с вторичным бесплодием как в общей выборке, так и для ОАТ-синдрома были старше, чем с первичным бесплодием и фертильные (табл.2; p<0,001), но разница составляла всего 3,9–4,4 года.
У фертильных мужчин В обнаружено в 27,2% случаев, в т.ч. первая – в 18,8%, вторая – в 7,6%, и третья – в 0,8%. Различия по сравнению с фертильными у мужчин из бесплодных пар значимы только для частоты случаев В второй степени в подгруппе с ОАТ-синдромом и вторичным бесплодием (ОШ=2,1; p<0,02).
Сведения о средних значениях показателей спермограммы и распростренности отдельных диагнозов (олиго-, астено-, тератозооспермия и др.) у мужчин с разной степенью В представлены в табл. 3.
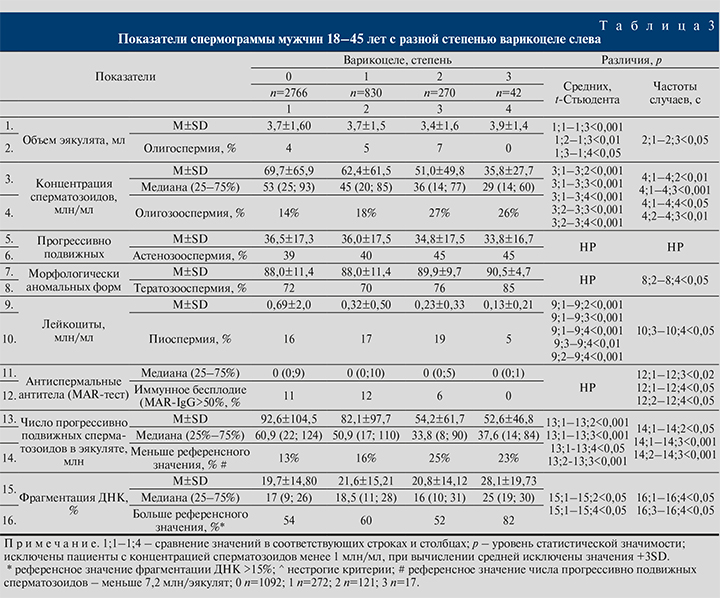
Объем эякулята пациентов с В в среднем не отличался от тех, у кого В не было (p>0,05), случаи олигоспермии в обоих случаях были редкими: 4% в отсутствие В и 0–7% при В разных степеней; но между группами с В имелись небольшие, но значимые различия (табл. 3).
Концентрация сперматозоидов существенно меньше во всех группах с В, и чем больше степень В, тем меньше средняя концентрация (табл. 3). Наблюдаемые изменения были высокодостоверны для всех сравниваемых групп (p<0,001); параллельно росло число случаев олигозооспермии: с 14% в группе без В до 27 и 26% в группах второй и третьей степеней (p<0,05-0,01). Сравнение медиан (распределение значений концентрации существенно отличается от нормального) показало (рис. 2), что при В первой степени концентрации меньше на 8 млн/мл (p<0,001), чем у мужчин без В, при второй – на 17 (p<0,001), при третьей – на 24 млн/мл (p<0,001). Различия в концентрации между группами с разной степенью В значимы (табл. 3, рис. 2): при второй и третьей степенях концентрация сперматозоидов меньше, чем при первой, на 6 (p<0,001) и 16 млн/мл (p<0,01) соответственно; чаще при этом наблюдается олигозооспермия (ОШ=1,44 и 1,5 соответственно; p<0,01). Различия между группами с второй и третьей степенями по распространенности олигозооспермии статистически не значимы (p>0,05).
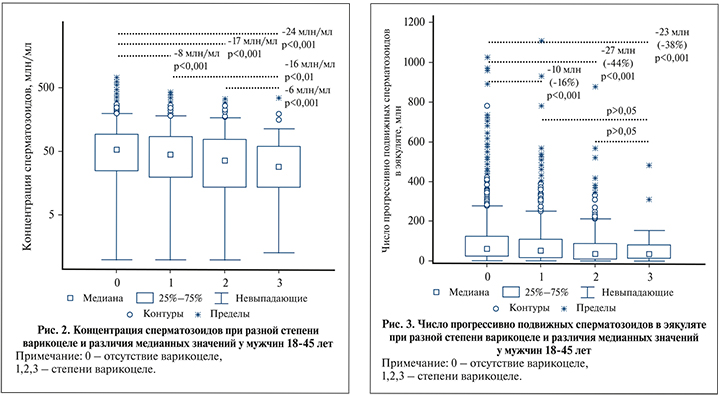
Процент прогрессивно подвижных сперматозоидов и распространенность астенозооспермии не значимы для всех сравниваемых групп (табл. 3; p>0,05). Но за счет различий в концентрации расчетное ЧППСЭ тем меньше, чем больше степень варикоцеле (табл. 3; p<0,5–0,001). Значение медианы данного показателя (рис. 3) при первой степени меньше на 10 млн (-16% по отношению к средней в группе без В; p<0,001), второй – на 27 (-44%; p<0,001), третьей – на 23 млн (-38%; p<0,001), но различия между группами с разной степенью В для ЧППСЭ не значимы (рис. 3; p>0,05).
Различия в проценте морфологически аномальных сперматозоидов и случаев тератозооспермии отсутствуют для всех групп (табл. 3; p>0,05), кроме увеличения распространенности тератозооспермии при В третьей степени по сравнению с первой (p<0,05).
Фрагментация ДНК сперматозоидов при В в среднем больше и встречается чаще (табл. 3; p<0,05), максимально выраженные изменения наблюдаются при третьей степени В (p<0,05).
Иммунное бесплодие (MAR-IgG>50%) чаще диагностировано у пациентов без В (табл. 3; р<0,05); при третьей степени АСАТ диагностированы реже, чем при первой (р<0,05).
Концентрация спермальных лейкоцитов была у пациентов с В меньше, чем без В (табл. 3; р<0,01–0,001); при второй и третьей степенях – меньше, чем при первой (р<0,01).
Обсуждение. Из результатов обследования 3632 мужчин из бесплодных пар и 276 фертильных мужчин следует, что наличие клинического В сопровождается уменьшением концентрации и качества сперматозоидов, что соответствует выводам многих опубликованных работ [4,6–10, 14, 25, 26]. По сравнению с мужчинами без В медиана концентрации, по нашим данным, при I ст. меньше на 8 млн/мл, II – на 17, III – на 24 млн/мл. Однако сила корреляционной зависимости между степенью В и концентрацией для всех обследованных групп весьма слаба: от -0,10 до -0,15; клинически значимое снижение концентрации – олигозооспермия – диагностировано только в 18–27% случаев В. Тот факт, что у большинства мужчин с В спермограмма соответствует диагнозу «нормозооспермия», отмечали многие исследователи [10, 11, 15, 16]. Расчет ЧППСЭ показал, что этот показатель снижен у мужчин с В, но различия между группами с разной степенью В незначимы. Ухудшение качества сперматозоидов, признаком чего является увеличение процента аномальных форм и фрагментации ДНК, описанное некоторыми исследователями [7, 8, 26], по нашим данным, становится статистически значимым только при третьей степени В.
Взаимосвязь В и аутоиммунных реакций против сперматозоидов была предметом анализа в одной из наших публикаций ранее [27].
Наши данные о распространенности В у мужчин из бесплодных пар и в целом и при первичном бесплодии близки к опубликованным: 28,1% в общей выборке и 31,4% при ОАТ-синдроме. Это несколько чаще, чем в одних работах [2, 13], и реже, чем в других [4, 28, 29]. Но при этом мы не обнаружили доминирования В у мужчин с вторичным бесплодием (50–80%), о чем писали некоторые авторы в 1990-е гг. [2, 30, 31] и что нередко цитируют до сих пор [29]. По нашим данным, у мужчин из вторично бесплодных пар клиническое В диагностировано в 31,6%, в т.ч. у 34,4% в случае ОАТ-синдрома. Различия могут быть связаны с тем, что мы не учитывали субклинических форм, а также с особенностями обследованной выборки (жители мегаполиса). Но главное, по нашему мнению, то, что в основе представления о столь высокой распространенности В при вторичном бесплодии лежат недостаточно корректные данные. В частности, в работе J. L. Gorelick, M. Goldstein [30] из 1099 бесплодных мужчин только 98 (9%) были с вторичным бесплодием и у 79 из них (81%) было диагностировано В (весьма малочисленная группа). Данные M. A. Witt и L. I. Lipshultz [31] более представительны: авторы оценили 2989 бесплодных мужчин и сообщили, что В идентифицировано у 69% мужчин с вторичным бесплодием. Но, как утверждают U. Levinger et al. [32], увеличение распространенности В у мужчин с вторичным бесплодием служит результатом возрастного увеличения распространенности В, так как эти мужчины, как правило, старше мужчин с первичным бесплодием [29, 32]. В нашей выборке различия в возрасте при первичном и вторичном бесплодии также были существенными, но составляли всего 3,9–4,4 года.
Оценить относительный риск развития бесплодия при В, по нашим данным, невозможно: распространенность В и отдельных стадий у фертильных мужчин и пациентов из бесплодных пар статистически не различаются: 27,2 и 29,5%. Если считать, что распространенность В при вторичном бесплодии более показательна – качество спермы при В быстрее ухудшается со временем, то соотношение между распространенностью В при вторичном бесплодии по сравнению с первичным можно считать суррогатным маркером такого риска. Эта величина, по нашим данным, составляет 1,13, т.е. весьма мала.
По нашему мнению, полученные данные подтверждают точку зрения, согласно которой В не является независимым фактором риска бесплодия, а лишь значимым ко-фактором, приводящим к снижению фертильности при наличии неких дополнительных факторов риска генетической природы, повреждений и/или образа жизни. Эту точку зрения почти 20 лет назад высказал J. L. Marmar [34] – автор известной методики коррекции В. Из генетических и эпигенетических факторов риска можно выделить мутации и полиморфизмы генов FAM47C, ATPase1A4, HSPA2, SPA17 и APOA1 и др. [35,36], из приобретенных – развитие аутоиммунных реакций против сперматозоидов [27], ожирение и курение [10]. Поэтому лишь в части случаев и в весьма разной степени помогает операция.
Заключение. Из результатов выполненного нами клинико-лабораторного обследования 3632 мужчин из бесплодных пар и 276 фертильных мужчин следует, что В сопровождается уменьшением концентрации сперматозоидов пропорционально степени В: на 8, 17 и 24 млн/мл для ст. I, II и III соответственно по сравнению с мужчинами без В. При этом в ¾ случаев концентрация сперматозоидов остается в границах референсных значений. Расчетное ЧППСЭ при В меньше, чем без В, но различия между группами с разной степенью В не существенны. Ухудшение качества сперматозоидов, признаком чего является увеличение процента аномальных форм и фрагментации ДНК, становится статистически значимым только при третьей степени В. Зависимость количества и качества сперматозоидов от В слабая (R=0,08–0,11). Клиническое В несколько чаще (ОШ=1,13) встречается у мужчин из вторично бесплодных пар, чем с первичным бесплодием, но по сравнению с фертильными различия не существенны (31,6%, 28,1 и 27,2% соответственно); нет различий и для подгрупп с ОАТ-синдромом. Поэтому корректно оценить риск развития бесплодия при В невозможно. По нашему мнению, В является ко-фактором и приводит к бесплодию при наличии неких дополнительных факторов риска генетической природы и/или образа жизни. Изучение комплекса факторов, снижающих фертильность у пациентов с В, должно быть предметом дальнейших исследований.