Введение. Мочекаменная болезнь (МКБ) является одним из наиболее широко распространенных и склонных к рецидивированию хронических заболеваний. Большой вклад в этиологию заболевания вносят генетические факторы.
И хотя основная доля случаев МКБ имеет мультифакториальную природу, на сегодняшний день известно уже более 80 моногенных форм этой патологии [1]. У большинства (80%) пациентов с МКБ преобладают кальциевые конкременты, которые в 85–90% случаев представляют собой оксалатно-кальциевые уролиты [2]. В клинической практике определенные трудности представляет диагностика случаев МКБ, обусловленных гипероксалурией, вследствие многообразия ее форм. Гипероксалурию можно подразделить на два основных вида: первичную (наследственно обусловленную) и вторичную (возникающую на фоне влияния различных факторов внешней среды).
Первичная гипероксалурия (ПГ) – группа редких наследственных метаболических заболеваний с аутосомно-рецессивным типом наследования, характеризующаяся гиперпродукцией и чрезмерным выделением оксалатов с мочой, что приводит к быстрому развитию МКБ и хронической болезни почек (ХБП). Причиной развития ПГ служит нарушение функции генов, ответственных за метаболизм оксалатов. В зависимости от того, в каком гене произошла мутация, выделяют три типа ПГ. При ПГ 1-го типа описаны мутации гена AGXT, при ПГ 2-го и 3-го типов – мутации в генах GRHPR и HOGA1 соответственно. Все типы ПГ различаются возрастом манифестации, степенью тяжести клинических проявлений и подходом к лечению.
Впервые сообщение о ПГ было сделано C. Lepoutre в 1925 г., описавшим ребенка с многочисленными отложениями оксалата в почках [3]. В 1955 г. H. G. Dunn предложил термин «оксалоз» для обозначения состояния, при котором формируются отложения оксалата в органах и тканях при развитии ХБП. В 1957 г. H. E. Archer et al. впервые определили различие между первичной и вторичной гипероксалурией и предложили термин «первичная гипероксалурия» для описания нефрокальциноза, возникающего в раннем детстве [4]. C. J. Danpure и P. Jennings в 1986 г. установили, что в клетках печени больных ПГ 1-го типа полностью отсутствует пероксисомный фермент аланин-глиоксилатаминотрансферазы (АГТ) [5]. Позднее, в 1990 г., те же авторы показали, что мутации гена AGXT служат причиной дефицита фермента АГТ, приводящего к развитию ПГ 1-го типа [6].
Первичная гипероксалурия 2-го типа впервые описана в 1968 г. как L-глицериновая ацидурия [7]. Однако идентифицировать ген GRHPR, связанный с ПГ 2-го типа, удалось только в 1999 г. [8].
Первичная гипероксалурия 3-го типа впервые описана в 2010 г. R. Belostotsky et al., выявившими мутации в гене HOGA1 у пациентов с МКБ [9].
В 2008 г. был создан европейский консорциум по гипероксалурии – Oxal Europe [10], в который вошли восемь европейских стран: Франция, Германия, Италия, Нидерланды, Польша, Испания, Швеция и Великобритания. Результатом его работы стало создание базы данных пациентов с ПГ, в которой представлена клиническая, генетическая и биохимическая информация более чем о 526 больных ПГ [11].
Оценка частоты ПГ довольно сложна, поскольку большинство случаев заболевания выявляются поздно или не выявляются при жизни пациента. Так, в проведенном в США исследовании показано, что 42% случаев ПГ диагностируются с существенным опозданием, у 30% пациентов диагноз был поставлен только после развития терминальной почечной недостаточности [12].
Данные о частоте ПГ в различных странах мира представлены в таблице.
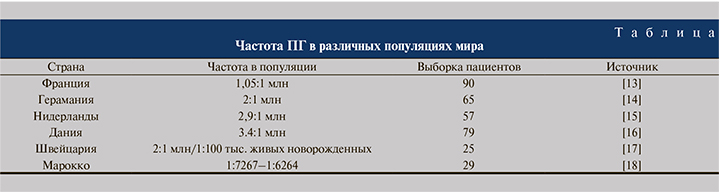
К сожалению, точные данные о частоте ПГ в России отсутствуют, до сих пор описаны лишь единичные клинические наблюдения. Однако по данным эпидемиологического исследования, проведенного в 1970–1980-х гг. (с охватом более 100 тыс. детей из 13 регионов России – от Ленинграда до Владивостока), встречаемость оксалатно-кальциевой кристаллурии составила 14:10 тыс. детской популяции [19].
Этиология и патогенез
Первичная гипероксалурия 1-го типа – наиболее тяжелая форма и встречается чаще остальных. Наследуется по аутосомно-рецессивному типу. Как уже было отмечено, ПГ 1-го типа обусловлена мутациями в гене AGXT, который расположен на хромосоме 2p37.3 и состоит из 11 экзонов. В данном гене описано более 150 мутаций, приводящих к развитию гипероксалурии с различной остаточной активностью фермента АГТ [11]. Около 75% описанных мутаций этого гена считаются точковыми, из них предположительно 73 миссенс-мутации, 19 нонсенс-мутаций и около 18 однонуклеотидных замен влияют на консенсусные последовательности сайта сплайсинга. Остальные 25% мутаций представлены делециями и дупликациями короткого плеча хромосомы 2 [20].
К наиболее распространенным в европейских и северо-американских популяциях относится мутация c.508G>A (p.Gly170Arg) гена AGXT, которая выявляется в 25–40% случаев ПГ 1-го типа [21]. Мутация c.508G>A (p.Gly170Arg) гена AGXT в гомозиготном состоянии связана с ответом на лечение пиридоксином, позже подобный эффект был выявлен для мутаций c.454T>A (p.Phe152Ile)и c.731T>C (p.Ile244Thr) этого гена [3]. Мутация c.731T>C(p.Ile244Thr) – вторая по частоте мутаций в гене AGXT и выявляется примерно среди 9% пациентов с ПГ 1-го типа. Остальные миссенс-мутации в гене AGXT встречаются гораздо реже [22].
Исследования M. B. Coulter-Mackie [23] показали, что мутация c.731T>C (p.Ile244Thr) гена AGXT чаще встречается среди людей, имеющих испанское или северо-африканское происхождение, также частота этой мутации высока среди популяции Канарских островов, что, вероятно, связано с эффектом основателя. Еще одной частой мутацией гена AGXT является мутация c.33_34insC (p.Lys12fs) с аллельной частотой около 13% среди всех аллелей ПГ 1-го типа в различных популяциях.
Таким образом, ПГ 1-го типа развивается вследствие мутаций гена AGXT, приводящих к снижению активности фермента АГТ, кофактором которого является пиридоксальфосфат, локализованный в пероксисомах гепатоцитов. Аланин-глиоксилат-аминотрансфераза метаболизирует глиоксилат, образующийся в процессе метаболизма гликольадегидов, в глицин и пируват. При нарушении работы АГТ происходит накопление глиоксилата, который превращается в оксалат посредством оксидазы гидроксикислот-1 в пероксисомах и лактатдегидрогеназы (ЛДГ) в цитозоле гепатоцитов [24].
Поскольку у млекопитающих оксалат не связывается с белками и не растворяется, он выводится в неизменном виде почечными клубочками и частично канальцами. Повреждение ткани почек связано с тем, что кристаллы оксалата, образуясь в почечных канальцах, становятся субстратом для агрегации кристаллов, выделяемых с мочой, и центром роста камней. Прикрепляясь к эпителиальным клеткам канальцев почек, кристаллы оксалата вызывают воспалительную реакцию, дегенеративные изменения и фиброз почечных тканей, с течением времени приводя к развитию ХБП. При развитии почечной недостаточности кристаллы оксалата кальция начинают накапливаться во внутренних органах, обусловливая системный оксалоз.
Первичная гипероксалурия 2-го типа (L-глицеровая ацидурия) возникает вследствие муциций в гене GRHPR, которые приводят к дефициту фермента глиоксилатредуктазы/гидроксипируватредуктазы. Ген GRHPR расположен в центромерной области хромосомы 9 (9p13.2) и состоит из 9 экзонов. На данный момент описано около 30 мутаций гена GRHPR [20]. Практически все мутации, описанные при ПГ 2-го типа, непосредственно влияют на кодирование или сплайсинг. Наиболее распространенной является мутация c.103delG (p.Asp35Thrfs*11) в экзоне 2 гена GRHPR. Она выявляется примерно в 40% случаев ПГ 2-го типа и приводит к сдвигу рамки считывания с формированием преждевременного стоп-кодона [25]. K. E. Webster et al. [26] пришли к заключению, согласно которому частота мутации c.103delG (p.Asp35Thrfs*11) гена GRHPR связана с эффектом основателя и имеет северо-европейское происхождение.
D. P. Cregeen et al. [27] сообщили, что данная мутация также была наиболее частой: в их когорте обследованных она обнаруживалась в 37% случаев и выявлена у 58% пациентов кавказского происхождения, но ее не удалось обнаружить ни у одного пациента азиатского происхождения.
В этом исследовании показано, что частота небольших делеций и инсерций в гене GRHPR выше, чем предполагалось ранее. В 2014 г. Y. Fu et al. [25] описали новую мутацию гена GRHPR – c.694delC (p.Gln232Argfs*3), которая приводила к формированию укороченной белковой молекулы с отсутствующей каталитической активностью. В том же исследовании обнаружено два генных варианта в 5′-UTR – c.-4G>A и c.-3C>T, которые вводят новый сайт трансляции, приводящий к сдвигу рамки считывания.
Мутации гена GRHPR обусловливают дефицит фермента глиоксилатредуктазы, функционирующего в основном в цитозоле гепатоцитов. При нарушении функции данного фермента происходит накопление глиоксилата и гидроксипирувата, которые превращаются в оксалат и L-глицерат с помощью ЛДГ [7]. При данной форме гипероксалурии оксалаты накапливаются в меньшем количестве и реже приводят к развитию терминальной почечной недостаточности, чем при ПГ 1-го типа.
Первичная гипероксалурия 3-го типа связана с мутациями, нарушающими функцию гена HOGA1. Данный ген расположен в районе 10q24.2 хромосомы 10 и состоит из 7 экзонов. Кодируемая им 4-OH-2-оксоглутаратальдолаза (ГОГ) преимущественно синтезируется в митохондриях гепатоцитов и клеток почек. Данный митохондриальный фермент участвует в метаболическом пути гидроксипролина и катализирует конечную реакцию – расщепление 4-гидрокси-2-оксоглутаратадо пирувата и глиоксилата. Мутации в гене HOGA1 приводят к накоплению ГОГ в крови, печени и выделению с мочой.
По данным литературы, для гена HOGA1 описано 26 патогенных вариантов мутаций, ответственных за развитие ПГ 3-го типа. В основном это миссенс-мутации и делеции со сдвигом рамки считывания, которые приводят к укорочению конечной молекулы белка, нарушению фолдинга, утрате стабильности молекулы и последующей целенаправленной деградации. Из них два наиболее распространенные мутации гена HOGA1 – c.700+5G>T и c.944_946del (p.Glu315del) – встречаются более чем у 70% пациентов с ПГ 3-го типа, при этом мутация c.700+5G>T составляет около 60% всех случаев [20]. Мутация c.944_946del (p.Glu315del) гена HOGA1 часто встречается у евреев-ашкенази [9].
В 2016 г. S. M’dimegh et al. [28] сообщили, что в тунисской популяции у троих пациентов с ПГ 3-го типа выявлены мутации c.569C>T (р.Pro190Leu) и c.860G>T (p.Gly287Val) в гене HOGA1. Выявленный у тунисского пациента патогенный вариант мутации c.569C>T (р.Pro190Leu) этого гена в гомозиготном состоянии был характерен только для жителей арабских стран, таких как Ливан, в связи с чем исследователи предположили, что арабская природа данной мутации связана с исторической миграцией населения [28]. Также были опубликованы данные о двух ранее не описанных мутациях в гене HOGA1, выявленных у ребенка из Китая. Первая мутация c.834_834+1GG>TT – замена двух пар оснований последнего нуклеотида экзона 6 и первого нуклеотида 6-го интрона, что приводит к нарушению сплайсинга и пропуску экзона 6. Вторая мутация c.834G>A представляет собой синонимичную замену, нарушающую процесс плайсинга [29].
Состав и морфология камней при ПГ
Обследование пациентов с ПГ 1-го типа показало, что камни в основном состоят из чистого моногидрата оксалата кальция (CaOx), иногда с примесью дигидрата CaOx.
В некоторых случаях возможно сочетание оксалата кальция и фосфата кальция [30]. В 2008 г. M. Daudon et al. [31] опубликовали данные исследования камней от 74 пациентов с ПГ 1-го типа. Авторы пришли к следующему заключению: при ПГ 1-го типа образуются камни с характерной морфологией, которая включает белую или бледно-желтую поверхность и рыхлую, неорганизованную внутреннюю структуру, в то время как камни, состоящие из моногидрата кальция при других нефролитиазах, имеют темно-коричневую поверхность и компактно организованную в виде лучей внутреннюю структуру, которая состоит из органического ядра и кристаллической мантии. D. E. Jacob et al. [32] получили несколько иные результаты. Они обнаружили, что у пациентов без лечения основным компонентом камней является дигидрат оксалата кальция, причем камни при ПГ 3-го типа могут быть неоднородными по внешнему виду и составу. В таких камнях дигидрат CaOx образует рыхлые агрегаты и демонстрирует большую вариацию в размере кристаллов, а моногидрат CaOx встречается только в междоузлиях кристаллов или в виде угловых кристаллов, связывающих молекулы дигидрата CaOx. Моногидрат оксалата кальция был основным компонентом камней у пациентов, находящихся на лечении цитратом в сочетании с витамином B6 или магнием [32]. Замещение дигидрата моногидратом CaOx вызвано тем, что дигидрат имеет более высокую растворимость и термодинамически менее стабилен, поэтому заменяется термодинамически более стабильным моногидратом CaOx [33].
Клиническая характеристика ПГ
Самым частым клиническим проявлением ПГ является МКБ, которая на момент установления диагноза имеет место у 90% пациентов. У значительной части пациентов диагноз устанавливают уже на стадии терминальной почечной недостаточности, у некоторых из них гипероксалурия диагностируется только после рецидива нефрокальциноза аллотрансплантата почек [12].
При ПГ 1-го типа средний возраст манифестации заболевания составляет 5 лет (диапазон с 1-го месяца жизни до 6-го десятилетия), а средний возраст смерти – 21 год [20].
В случае манифестации ПГ 1-го типа в первые месяцы жизни у пациентов развиваются признаки уремии: слабость, вялость, тошнота, рвота, бледность. При инструментальном обследовании может быть выявлен нефрокальциноз или системный оксалоз в тяжелых случаях. У 65% пациентов симптомы гипероксалурии проявились до 10, у 85% – до 20 лет. Более чем у 50% больных ХБП развивается к 25 годам жизни, 28% из них требуется заместительная почечная терапия (диализ/трансплантация почки) уже к 15 годам [34]. При прогрессировании ХБП и достижении критического уровня оксалата в плазме кристаллы оксалата кальция начинают накапливаться в различных тканях: сердце, суставах, костях, коже, мягких тканях и сетчатке. Данное осложнение носит название системного оксалоза. Оно возникает в результате снижения скорости клубочковой фильтрации (СКФ), что приводит к накоплению оксалата в плазме крови в концентрациях, превышающих пороговый уровень насыщения, и осаждению оксалата в тканях с развитием в них воспалительной реакции. Осаждение кристаллов оксалата прежде всего происходит в тканях, богатых кровеносными сосудами.
В литературе описаны случаи поражения глаз, главным образом сетчатки, цилиарного тела и глазных мышц, костей с развитием болей в костях, патологических переломов и костных деформаций, в тяжелых случаях формируются субпериостальные тофусы [35, 36]. Следствием поражения костного мозга служит развитие вторичной анемии, резистентной к лечению эритропоэтином, в некоторых случаях может развиваться панцитопения [37]. Отложения кристаллов в пульпе зубов, альвеолярных отростках становятся причиной зубной боли, гиподонтии, микродонтии и периодонтита [38]. При развитии системного оксалоза патологический процесс также затрагивает сердечно-сосудистую систему. У пациентов могут наблюдаться гипертрофия миокарда и кардиомиопатия, приводящие к развитию сердечной недостаточности, кроме того, отложение оксалатных депозитов может обусловливать нарушение деполяризации кардиомиоцитов и проводимости сердечной мышцы с развитием фибрилляции желудочков [39]. Помимо этого ввиду отложения оксалатов в просвете сосудов и повреждения сосудистой стенки развивается эндотелиальная дисфункция, обусловливающая микроциркуляторные нарушения [40]. В литературе описано несколько случаев ишемических инсультов, вызванных нарушением микроциркуляции и тромбоэмболией кристаллами оксалата кальция [41]. К осложнениям оксалоза в результате эндотелиальной дисфункции также относятся кожные проявления в виде акроцианоза, сетчатого ливедо, булл и некротических язв дистальных отделов конечностей c развитием фиброза тканей [42]. Поражение нервной системы при оксалозе чаще проявляется в виде периферической полинейропатии [43]. В качестве осложнения системного оксалоза со стороны эндокринной системы описано развитие гиперкальциемии и гипотиреоза [44]. Для этого типа гипероксалурии характерна высокая смертность в раннем возрасте.
Первичная гипероксалурия 2-го типа практически не отличается от ПГ 1-го типа ни по возрасту манифестации, ни по уровню оксалата в плазме, поэтому очень сложно бывает провести дифференциальную диагностику. Манифестирует заболевание чаще в детском возрасте. Как правило, первым проявлением является МКБ.
В отличие от ПГ 1-го типа пациенты с ПГ 2-го типа имеют более длительную продолжительность жизни, а терминальная стадия ХБП и оксалоз развиваются в более старшем возрасте [45].
Первичная гипероксалурия 3-го типа встречается реже и проявляется более легкой клинической картиной, характеризующейся нефролитиазом в зрелом возрасте, не прогрессирующим до ХБП. Первичная гипероксалурия данного типа чаще всего манифестирует в детском возрасте.
К первым проявлениям заболевания в ряде случаев относятся МКБ, гематурия, почечная колика, мочевая инфекция [3]. Большинство пациентов с ПГ 3-го типа имеют нормальную СКФ, и терминальная стадия ХБП не развивается, однако описаны случаи нарушения функции почек и снижения СКФ у пациентов при сочетании мутаций в обоих аллелях гена HOGA1 с гетерозиготным носительством мутации в гене AGXT [46]. Системный оксалоз при данной форме не описан. Опубликовано довольно много работ, в которых исследователи пытались определить четкую корреляцию генотипа с фенотипом. К сожалению, на сегодняшний день этот вопрос остается открытым [20].
Первичная гипероксалурия характеризуется широкой клинической гетерогенностью, различным возрастом манифестации и отсутствием строгой генофенотипической корреляции. Настороженность профильных специалистов, особенно педиатров, и ранняя молекулярно-генетическая диагностика необходимы для быстрой постановки клинического диагноза и выбора оптимальной тактики лечения пациента. Знание молекулярных механизмов, лежащих в основе патогенеза МКБ, позволяет разработать новые более эффективные методы лечения и метафилактики. Кроме этого на основе уже накопленных знаний о патогенезе проходят испытания новые методы патогенетической терапии: ферментозаместительная, субстрат-редуцирующая и этиологическая терапия, генотерапия с применением вирус-ассоциированных векторов [47, 48].