Данные о новой коронавирусной инфекции противоречивы, однако пандемия уже диктует множество репродуктивных ограничений. Распространение SARS-CoV-2 привело к остановке работы клиник вспомогательных репродуктивных технологий (ВРТ), в первую очередь для снижения нагрузки на здравоохранение. Многие международные сообщества рекомендовали потенциальным родителям, пациентам и донорам избегать участия в программах репродукции и беременности. Позднее, признавая неотъемлемое право человека на размножение, были опубликованы рекомендации от профессиональных организаций по наилучшей практике анализа рисков, использования соответствующих средств индивидуальной защиты и мер социального дистанцирования [1, 2]. Некоторые исследователи предполагают, что демографические последствия прекращения работы репродуктивных служб могут быть сопоставимыми с потерями, связанными с пандемией [3].
Патофизиологические предпосылки вовлечения яичек
Основанием для беспокойства служит известная особенность SARS-CoV-2, как и всех представителей семейства коронавирусов, проникать в клетку хозяина, используя особые гликопротеины-«шипы» (S). Белок S имеет две субъединицы – S1 и S2. В то время как S1 связывается с ангиотензинпревращающим ферментом 2-го типа (АПФ2, ACE2), S2 активируется мембраносвязанной сериновой протеазой (TMPRSS2). ACE2 и TMPRSS2 используются вирусом как рецептор для проникновения и репликации в клетках [4, 5].
TMPRSS2 высоко экспрессируется в эпителиальных клетках предстательной железы, а также сперматогониях и сперматидах [6]. Экспрессия ACE2 обнаружена в сперматогониях, клетках семенных канальцев, клетках Лейдига и необычайно высока в клетках Сертоли, участвующих в формировании гематотестикулярного барьера (ГТБ). Предполагается, что клетки Сертоли наиболее восприимчивы к воздействию инфекции SARS-CoV-2 [4, 7]. Физиологические функции ACE2 в клетках Лейдига включают регуляцию продукции тестостерона и объема интерстициальной жидкости путем модулирования превращения ангиотензина II в ангиотензин I [8].
C. Song et al. [5] предполагают, что SARS-CoV-2 вряд ли проникает в клетки яичка человека. Необходимым условием доступа вируса к клетке является присутствие на ней обоих рецепторов – ACE2 и TMPRSS2. Гены, кодирующие эти два белка, были выявлены только в 4 из 6500 исследованных клеток яичка, что стало подтверждением их гипотезы с определенными ограничениями [5].
Молодые мужчины репродуктивного возраста подвержены большему риску повреждения тестикулярной ткани вследствие COVID-19. С возрастом и при наличии серьезных нарушений сперматогенеза наблюдается снижение экспрессии ACE2 в клетках Сертоли [7]. Наибольшая экспрессия регистрируется у мужчин в возрасте 20–30 лет, минимальная – в возрасте 60 лет [9]. Таким образом, новая коронавирусная инфекция может влиять как на соматические клетки яичка, участвующие в производстве сперматозоидов, так и непосредственно на половые клетки и их предшественники. Снижается ли экспрессия ACE2 у мужчин после перенесенной коронавирусной инфекции, еще предстоит выяснить. Также неизвестно, запускает ли COVID-19 высвобождение ACE2 с поверхности сперматозоидов или их предшественников и приводит ли потеря этого фермента к их гибели? С учетом вовлечения ГТБ открыт вопрос вирус-ассоциированного воспалительного повреждения ткани яичка (иммунного орхита) и появления антиспермальных антител (АСАТ), приводящих к иммунологическому мужскому бесплодию.
Клинические данные
Несмотря на не слишком оптимистичные патофизиологические предпосылки, клинические данные по обнаружению вируса непосредственно в ткани яичка и эякуляте обнадеживают.
Наличие вируса в эякуляте
Выделение вируса определяет инфекционный статус пациента. В настоящее время клиническая практика сосредоточена главным образом на идентификации коронавируса в назо/орофарингеальных (НФ) мазках и мало что известно о его присутствии в других средах организма. РНК SARS-CoV-2 обнаруживалась в низких титрах в кале, моче и крови человека. Процент пациентов с наличием вирусной РНК в моче и крови представляется довольно низким [10].
Виремия рассматривается как одна из основных причин положительных образцов спермы. Гематотестикулярный барьер служит несовершенной преградой для проникновения инфекции, особенно при наличии системного или местного воспаления. Известно более чем о 27 вирусах различных семейств, способных вызывать виремию, и как минимум 11 из них обнаруживаются в яичках. Одни размножаются в мужском репродуктивном тракте, другие могут сохраняться годами в клетках или секретах в виде свободных частиц [11]. Стоит также учитывать, что не все лекарственные средства преодолевают ГТБ и вирусы могут сохраняться в сперме, несмотря на системный клиренс. Более высокая вирусная нагрузка связана с более тяжелыми симптомами заболевания, и вполне вероятно, что должен быть преодолен определенный вирусный порог для выявления SARS-CoV-2 в эякуляте, как это происходит в случае с ВИЧ [11].
Что касается COVID-19, исследований немного (см. таблицу). Наличие РНК в эякуляте было подтверждено только в одной работе [12], в которой, однако, отсутствовало описание процедуры сбора образцов. Получение материала путем мастурбации трудно назвать стерильной процедурой и нельзя исключить попадания вируса при дыхании или с рук. Чтобы избежать заражения вирусом из других источников, процесс должен включать мочеиспускание, тщательное мытье рук и полового члена с мылом, их сушку, а затем эякуляцию спермы в стерильный контейнер с широким горлышком [5].
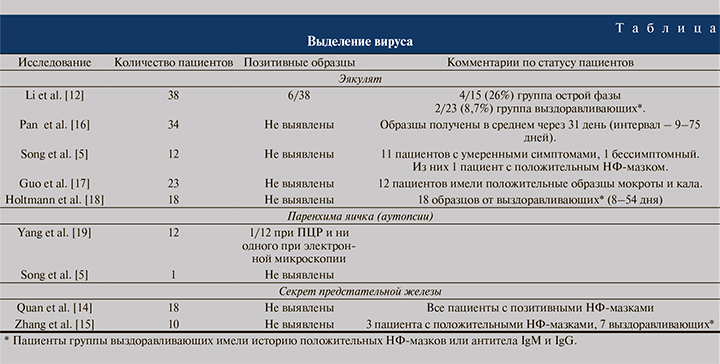
Секрет простаты составляет примерно треть общего объема спермы и потенциально может служить резервуаром для коронавируса. Известно, что простата экспрессирует ACE2 и TMPRSS2 [13], что не исключает вероятности вовлечения железы и выделения вируса из секрета, однако клинически это пока не было подтверждено [14, 15]. По мнению C. Song et al. [5], маловероятно, что SARS-CoV-2 может непосредственно инфицировать яички или половые пути мужчины и передаваться половым путем.
SARS-CoV-2, как и вирус гриппа, является РНК-вирусом с оболочкой, поэтому может оставаться жизнеспособным при оттаивании после криоконсервации.
В связи с этим были разработаны усиленные меры предосторожности для криобанков [1, 2, 20] с использованием высокозащищенных устройств и отдельных криососудов. Очень низкие титры SARS-CoV-2 в нереспираторных тканях (кал и моча) также поддерживают гипотезу о малой вероятности присутствия вируса в семенной плазме [10, 20]. Тем не менее даже незначительный риск неприемлем в свете лечения здоровых пар в бесплодном браке.
Орхит и гистопатология
Классические симптомы орхита при COVID-19 не описаны. Фактически о дискомфорте в органах мошонки заявлено только в одном исследовании, где 6 (19%) из 34 мужчин испытывали этот симптом, но никакого андрологического обследования по этому поводу не проводилось и диагноз орхита не был подтвержден [16].
В небольшой серии аутопсий (n=12) пациентов с COVID-19 были выявлены значительные повреждения паренхимы яичек, уменьшение количества клеток Лейдига и невыраженное лимфоцитарное воспаление. Среднее количество клеток Лейдига в яичках было значительно ниже, чем в контрольной группе (2,2 против 7,8; р<0,001). Средний возраст составил 65 (42–87) лет. Несмотря на то что группой контроля служили 5 мужчин, средний возраст которых был составлял 66,8 (49–75) года, следует учитывать, что количество клеток Лейдига значительно снижается с возрастом, а возраст пациентов исследуемой группы несколько выходит за рамки репродуктивных интересов [19].
Аналогичные данные, соответствовавшие гистопатологической картине орхита, получены в небольшой контролируемой серии (n=6) пациентов с близкородственным COVID-19 вирусом SARS-CoV-1 (SARS), эпидемия которого была успешно ликвидирована в 2003 г. Примечательно, что в этом исследовании возраст мужчин гораздо больше соответствовал репродуктивным интересам – в среднем 39 лет (от 20 до 58 лет). Исследователи выявили обширное повреждение герминогенных клеток, небольшое количество или отсутствие сперматозоидов в семенных канальцах, утолщенную базальную мембрану и инфильтрацию лейкоцитов в отсутствие вируса in situ. При иммуногистохимическом исследовании обнаружено обильное осаждение IgG в семенном эпителии яичек пациентов с SARS, что указывает на иммунный ответ как на возможную причину повреждения канальцев [21].
Вполне вероятно, что иммуносупрессивные свойства клеток Сертоли и макрофагов яичка могут играть критическую роль в подавлении воспаления и ограничении связанного с вирусом повреждения яичка в отличие от других органов, что проявляется гистопатологической картиной орхита. Воспаление, связанное с SARS-CoV-2, может временно нарушать целостность ГТБ, что может стать в последующем причиной бесплодного брака [22]. Не исключено, что орхит может быть результатом васкулита, так как COVID-19 ассоциирован с нарушениями коагуляции, а сегментарная васкуляризация яичка может обусловливать возникновение синдрома, подобного орхиту [20].
Гипогонадизм
Гистологически ыявленное снижение количества клеток Лейдига [19] находит косвенные подтверждения в клинических докладах. Так, у мужчин с уровнем общего тестостерона менее 5 нмоль/л наблюдалось резкое увеличение как вероятности нахождения в отделении интенсивной терапии, так и риска смерти [23]. Связь мужских гормонов с тяжестью течения инфекционного процесса была показана в другой работе. Низкие уровни тестостерона и дигидротестостерона при обследовании 35 мужчин из отделения интенсивной терапии были зарегистрированы в 68,6 и 48,6% случаев соответственно [24].
L. Ма et al. представили результаты обследования 81 мужчины репродуктивного возраста с инфекцией SARS-CoV-2 и 100 здоровых мужчин соответствовавшего возраста. Уровни тестостерона в сыворотке крови в группах не различались. При этом содержание сывороточного лютеинизирующего гормона (ЛГ) было значительно повышено, тогда как соотношение тестостерона и ЛГ и соотношение фолликулостимулирующего гормона и ЛГ у мужчин с COVID-19 было резко сниженным, что свидетельствует о возможном гипогонадизме. Авторы предупредили о необходимости оценки гормональной функции у инфицированных мужчин репродуктивного возраста [25].
Тем не менее о каких-либо неблагоприятных исходах можно рассуждать по крайней мере через 3–6 мес. после выздоровления. В настоящий момент трудно достоверно определить причинно-следственную связь. Снижение и изменение гормонального фона могут быть вызваны тяжестью заболевания, сопутствующей патологией, вовлечением яичек в инфекционный процесс или же быть первичным по отношению к инфекции, увеличивая риск тяжелого течения заболевания. Стоит учитывать вероятность вторичного гипогонадизма, поскольку известно о наличии ACE2 в головном мозге, возможности проникновения SARS-CoV-2 через гематоэнцефалический барьер, а также о возникающих психоневрологических нарушениях на фоне болезни [27].
Качество спермы
Исследование, оценивавшее параметры эякулята у 23 мужчин 20–62 лет, не выявило никаких отклонений в общем количестве сперматозоидов, общем количестве подвижных сперматозоидов и их морфологии при обследовании через 1 мес. после обнаружения SARS-CoV-2 [17]. В другой работе по результатам обследования 20 мужчин с новой коронавирусной инфекцией выявлены статистически значимые различия показателей объема, полной подвижности и количества неподвижных сперматозоидов по сравнению с контролем (морфология не оценивалась), при том что все эти значения находились в пределах нормы [18].
Многие шутливо высказываются о предстоящем «бэби-буме» после периода самоизоляции. Между тем высока вероятность диаметрально противоположных последствий социального дистанцирования даже для тех, кто не переболел COVID-19. Остановка оказания плановой помощи, отсутствие физической активности, стресс, тревожные и депрессивные расстройства, расстройства пищевого поведения, нарушения сна — все это влияет на общее состояние здоровья, микроклимат в паре и количество половых контактов [27, 28].
Окислительный стресс
В физиологических условиях окислительно-восстановительный баланс поддерживается ферментативными и неферментативными системами и способствует регуляции некоторых функций клеток. Вирусы нарушают это равновесие и вызывают окислительный стресс (ОС), который в свою очередь облегчает определенные этапы жизненного цикла вируса и активирует воспалительную реакцию. Индукция ОС посредством различных механизмов типична как для ДНК-, так и для РНК-вирусов. Избыточное накопление активных форм кислорода (АФК) регистрируется при многих вирусных инфекциях (гепатит В и С, лихорадка денге, грипп, ВИЧ и др.) [29, 30]. Сообщается, что ОС и нарушение функционирования антиоксидантных систем связаны с патогенезом и тяжестью новой коронавирусной инфекции [31].
Проведя анализ литературы, M. Alpalhao et al. [32], представили три пути нарушения окислительного равновесия у пациентов с COVID-19. В первую очередь SARS-CoV-2, связываясь с ACE2, блокируют его антигипертензивную, противовоспалительную, антифиброзную и антиоксидантную активность. Другой важный игрок – макрофаги, которые служат источником АФК. Третьим источником АФК может быть названо непосредственно лечение и повреждение ткани легких. Также исследователи предполагают, что эндотелиальная дисфункция сопровождает COVID-19 и сдужит основным источником АФК [33].
К ОС-опосредованным механизмам мужского бесплодия относят изменения основных параметров эякулята, нарушение функции и морфологии сперматозоидов, повреждение мембран и ДНК, а также индукцию апоптоза половых клеток [34, 35]. Как уже отмечено выше, вирус может вызывать орхит, который также может индуцировать ОС. Стимулируют высвобождение АФК и усугубляют последующую фрагментацию ДНК лекарственные препараты, например рибавирин, и даже психологический стресс [35].
Фрагментация ДНК ситается важным этиологическим фактором мужского бесплодия, основной причиной которого остается ОС, однако рутинное использование диагностических тестов все еще обсуждается. Мужчины с высоким уровнем фрагментации ДНК имеют более низкие шансы зачатия естественным путем или с помощью внутриматочной инсеминации и экстракорпорального оплодотворения [36]. В условиях новой пандемии внимание исследователей должно быть обращено не только на параметры эякулята, но и на фрагментацию ДНК сперматозоидов, которая должна быть исследована и по возможности сведена к минимуму. Снижение ОС может улучшить шансы пары на зачатие либо естественным путем, либо посредством вспомогательной репродукции [38].
Полноценность иммунного ответа зависит от характера питания, например достаточное потребление белка, в частности глютамина, аргинина и аминокислот, имеет решающее значение для продукции антител. Низкий уровень питательных микроэлементов связан с повышенным риском заражения [30]. Помимо минеральных компонентов, таких как цинк и селен, следует подчеркнуть роль омега-3 жирных кислот и антиоксидантных витаминов, поскольку их действие направлено в первую очередь на минимизацию окислительного стресса и воспаления.
В связи с этим диета должна быть разнообразной и сбалансированной, включать овощи и фрукты, рыбу и морепродукты, орехи, семена, цельнозерновые продукты, птицу и молочные продукты с низким содержанием жира [30, 39]. Модели здорового и сбалансированного питания четко коррелируют с лучшим качеством эякулята и меньшим риском отклонений в его параметрах, таких как количество сперматозоидов, их концентрация и подвижность, а также более низкой фрагментацией ДНК сперматозоидов [38, 39].
Дополнительный прием антиоксидантов связывают с увеличением частоты клинических беременностей и живорождений [40]. Также в экспериментальных моделях иммунного орхита показана эффективность терапии с использованием антиоксидантов и противовоспалительных средств [41]. Выраженное снижение маркеров ОС на фоне приема антиоксидантов при их относительной безопасности и эффективности [40, 42] может стать предпосылкой к будущим исследованиям по применению антиоксидантной терапии мужчин репродуктивного возраста, перенесших COVID-19.
Основной проблемой, с которой сталкиваются при назначении антиоксидантных добавок при мужском факторе бесплодия, считается гетерогенность исследований, не позволяющая сформировать единые рекомендации. Предложено внушительное количество антиоксидантов и их комбинаций, изученных в исследованиях разного качества. На территории РФ одним из антиоксидантных комплексов с хорошей доказательной базой является АндроДоз, состоящий из 9 активных компонентов (L-аргинин, L-карнитин, коэнзим Q10, L-карнозин, витамины Е и А, цинк и селен в органической форме, глицирризиновая кислота). Комплекс достоверно улучшал базовые параметры эякулята [43–45], а также снижал фрагментацию ДНК у мужчин с варикоцеле [43] и улучшал исходы ВРТ (клиническая беременность) [45].
Длительная лихорадка
Лихорадка регистрируется у 43,8% пациентов с COVID-19, а среди госпитализированных пациентов – уже в 88,7% наблюдений [46]. Предыдущие исследования SARS-CoV-1 показали, что высокая температура способствует разрушению половых клеток [21]. Наиболее вероятный механизм — вторичный аутоиммунный ответ, запускаемый длительно сохраняющейся высокой температурой [47].
Отсутствие физической активности
В условиях пандемии SARS-CoV-2 из-за требований самоизоляции и карантина сформировались условия существенного ограничения физических нагрузок и преимущественно сидячего образа жизни, ассоциируемые с плохим физическим и психическим здоровьем, повышенным риском смерти [48]. Без последствий не проходят даже короткие периоды без нагрузки: двухнедельное сокращение ежедневного количества шагов с 10 тыс. до 1500 приводит к нарушению липидного обмена и чувствительности к инсулину, увеличению объема висцерального жира, снижению костно-мышечной массы и ухудшению функции сердечно-сосудистой системы у здоровых взрослых [49].
Показано, что основные медиаторы ожирения – инсулин, цитокины и адипокины – нарушают мужскую фертильность вследствие гормональных нарушений и метаболической дисрегуляции. Известно о негативном влиянии на параметры спермы, такие как концентрация сперматозоидов, их подвижность, жизнеспособность и нормальная морфология. Кроме того, при ожирении снижается конденсация хроматина, фрагментация ДНК, увеличиваются апоптоз и эпигенетические изменения, которые могут быть переданы потомству [50].
Снижение качества жизни
Постинфекционная астения – состояние, развивающееся после острого гриппоподобного заболевания и сопровождающееся необъяснимой постоянной или рецидивирующей усталостью, которая приводит к значительному снижению активности и сопровождается другими симптомами хронической астении. В МКБ-10 кодом G93.3 обозначен синдром утомляемости после перенесенной вирусной болезни. Зарубежные коллеги чаще употребляют термин «миалгический энцефаломиелит/синдром хронической усталости». Около 11% пациентов, перенесших инфекцию, вызванную вирусами гриппа, Эпштейна–Барр, Коксаки, имеют признаки этого синдрома. В то же время до 50% пациентов после SARS-CoV-1 заявляли об усталости, фибромиалгии, депрессивных симптомах и расстройствах сна [51]. Эмоциональная лабильность, нарушение концентрации внимания, усталость и нарушение памяти были зарегистрированы более чем у 15% пациентов после SARS в течение периода наблюдения от 6 до 39 мес. Это вызывает беспокойство, поскольку предполагается, что нарушения памяти, внимания, концентрации или когнитивных способностей могут наблюдаться спустя год после перенесенного COVID-19 [27], что представляет важный психосоциальный аспект бесплодного брака [28].
Поскольку сопутствующие заболевания оказывают значительное влияние на общий исход COVID-19, мужчины с разнообразными факторами, предрасполагающими к бесплодию, еще более уязвимы к SARS-CoV-2 [30]. Спасение жизни – первоочередная задача здравоохранения, а влияние SARS-CoV-2 на фертильность может быть изучено на выздоровевших пациентах. Поскольку воздействие этого вируса длительное, а цикл сперматогенеза составляет 70–75 дней, мы уверены, что в ближайшие 4–6 мес. появятся новые данные и могут быть сформированы единые рекомендации относительно безопасного планирования семьи в условиях пандемии.
Имеющиеся на сегодняшний день данные не позволяют полностью исключить непосредственного или отсроченного влияния COVID-19 или его терапии на мужскую фертильность, которая и без того демонстрирует глобальную тенденцию к снижению. По всей видимости, воспалительные и иммунологические реакции, в том числе вследствие ОС, могут играть ключевую роль в вирус-опосредованном вовлечении ткани яичка. Повреждение клеток яичка может быть вызвано либо непосредственно присутствием вируса в клетках с ACE2, либо местным воспалительным ответом, вторичным к инфекции. В обоих случаях поражение гонад может сопровождаться изменениями в сперматогенезе и эндокринной функции яичек и быть связанным с повышенным риском бесплодия, особенно для пациентов репродуктивного возраста. Несмотря на то что большинство предварительных работ указывает на низкий риск неблагополучных для репродуктивной функции исходов, следует быть очень осторожными в выводах. COVID-19 демонстрирует очень высокую вариабельность клинических проявлений и их тяжести, что обосновывает необходимость дальнейших исследований.